An excruciating headache and strange tingling in her legs told Cindy Nava something was seriously wrong.
But little did she suspect that when her husband took her to a local urgent care clinic last August 17 that within in a week she would be undergoing brain surgery at The University of New Mexico Hospital for removal of a benign cyst the size of a golf ball.
Months after the delicate three-hour procedure, led by UNM neurosurgeon Christian Bowers, MD, Nava is fully recovered and has resumed her daily runs and Pilates sessions.
The 34-year-old policy and political strategist was the picture of health before she noticed symptoms on Sunday, August 15. They subsided, but returned two days later with a vengeance while she was on a Zoom conference call.
“I turned off the camera,” Nava recalls. “It just got worse and it increased by the minute. My husband got here and he noticed I was not myself.”
He rushed her to an urgent care where she was finally seen after a long wait. The medical team thought she might be experiencing a severe migraine, but one young doctor, concerned about her report of leg tingling, ordered a CT scan.
“The doctor and another one came in and they were very serious,” Nava says. “He said, ‘Don’t get scared, but we found a tumor in your brain. We can’t necessarily tell the size – possibly the size of a large almond.’”
They sent her to Presbyterian Hospital, where additional MRI and CT imaging revealed that she had a colloidal cyst, a large non-cancerous growth, that obstructed the flow of cerebrospinal fluid in her brain. When these cysts are left untreated, patients may experience hydrocephalus, intermittent headaches, nausea and vomiting – and even die.
Presbyterian neurosurgeon Jose Santos, MD, described what surgery to remove the cyst would entail. “I was very nervous because he told me they would make a significantly large insertion to go in,” Nava says. “He talked about a shunt to drain the cyst into my stomach, which would stay in for rest of my life. It was very hard for my family.”
Santos told her the procedure was risky. “He said, ‘We can do the surgery here, but I want the best person to treat you and the most equipped team to do so,’” she says. “He told me that at the moment he was texting with a few other surgeons from across the state to see if there was any potential that anyone who was more equipped or had better tools to do it.”
Later, he returned with an alternative: Nava could transfer to UNMH, where Christian Bowers had experience using a new device that enables minimally invasive brain surgery. After three days at Presbyterian she moved to UNMH, where she underwent further testing in preparation for surgery on Monday, August 23.
As she awaited surgery, “All of the people I worked for or worked with were looking Dr. Bowers up,” she says. “Everybody kept telling me they were very impressed by his experience. Folks in my network were very reassured by his work.”
But at one point, “I just kind of broke down and I probably cried for about an hour,” Nava says. “There were two nurses who came over and started talking to me. They sat there until I calmed down. I think everything was very overwhelming – the risk, the unexpectedness. Everybody was very supportive.”
On the day of surgery Bowers and fellow neurosurgeon Heather Spader, MD, opened a 3-centimeter hole in Nava’s skull where her forehead met the hairline. Using a state-of-the-art device that navigates through the brain’s natural folds without damaging tissue, he was able to reach the cyst and suction it out.
When Nava woke after surgery Bowers was at her bedside. “He said, ‘It went great. We removed everything,’” she says. He also told her the cyst had been blocking cerebrospinal fluid from reaching her spinal cord, which explained the leg pain.
“He said more than likely I was born with it and it started growing,” Nava says. “He said clearly it was now at a point where it was damaging. Had it touched any other areas, that would have been a different story.”
Nava spent three more days in the UNMH Neurosciences Intensive Care Unit before leaving the hospital. And although she was sore and tired from the surgery, she asked Bowers whether she would be able to attend the weekend wedding of her friend and mentor U.S. Interior Secretary Deb Haaland.
“He said, ‘You know your body best – you can definitely make an appearance, but have somebody with you,’” she says. “I’m glad I got the approval.”
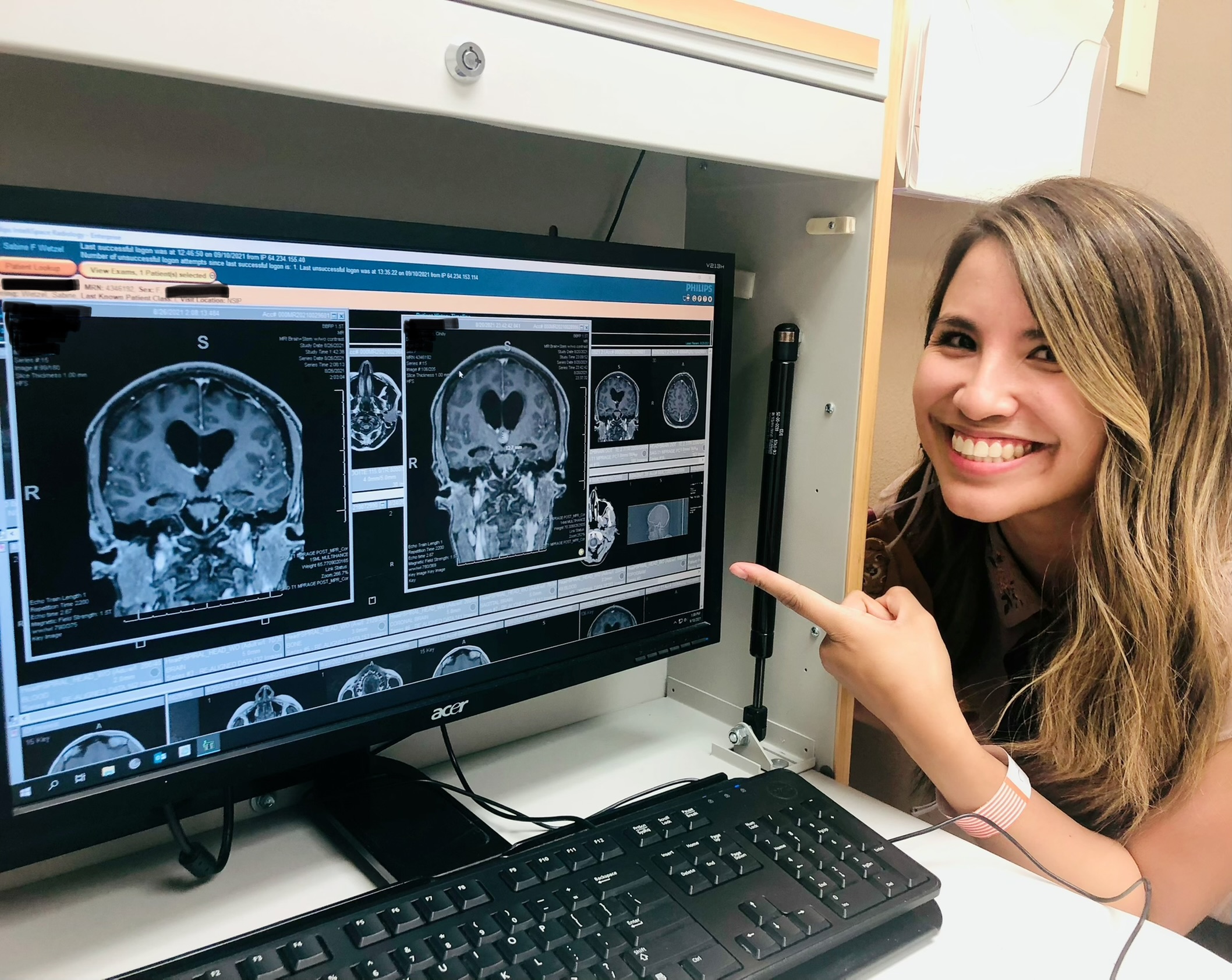
Over the next few weeks Nava found herself taking naps every day, and on her first post-operative appointment with Bowers, “He checked everything – he said everything looked great,” she says.
Nava is thankful for the skilled medical and nursing care she received at every step along the way.
Everyone played a vital role, but clearly the surgery itself was the thing that everybody was most nervous about because of the risks and how delicate it was.
“I think everyone played a vital role, but clearly the surgery itself was the thing that everybody was most nervous about because of the risks and how delicate it was,” she says. “I’m grateful for the technology, but I told Dr. Bowers for what it’s worth, this has clearly marked my life and I’m going to use this to tell a story.”
