New research at The University of New Mexico is helping patients in kidney failure, who endure hours of exhaustive, mentally draining dialysis each week, find better mental health outcomes.
Patients in kidney failure often use dialysis, a process where a machine replaces the function of the kidneys to filter waste and excess fluids from the blood. But undergoing dialysis often brings a high burden of other unpleasant symptoms – like fatigue, pain and depression – which are often outside a nephrologist’s wheelhouse in terms of treatment.
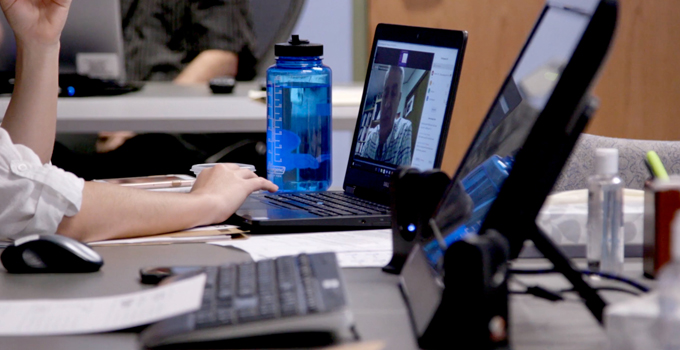
A new patient-guided intervention using telemedicine has been shown to improve these troublesome symptoms with beneficial results that persist for several months after the intervention ends, according to the results of a randomized clinical trial recently published in JAMA Internal Medicine by researchers at UNM and the University of Pittsburgh.
“This study was a true team effort,” said Mark Unruh, MD, MS, chair of the UNM School of Medicine Internal Medicine Department. “We saw patients from both New Mexico and Pennsylvania. It’s neat that New Mexicans will influence the care that everyone receives going forward.”
Nearly half a million people in the U.S. with end-stage kidney disease receive hemodialysis, where they are hooked to a machine, generally in a dialysis unit, at least three days a week for several hours. Many others use peritoneal dialysis, where the machine generally does it work while the patient sleeps at night at home.
“The symptom burden of folks who are being supported by dialysis is really high,” Unruh said. “Often, these symptoms are overlooked because we usually have a medical and disease-specific approach to managing patients and doing research.”
”When you talk to patients, they don’t necessarily tell you they want you to cure their kidney failure. More often than not, they want to know how to manage fatigue and pain or how to have a better mood and experience less anxiety,” Unruh added.

When you talk to patients, they don’t necessarily tell you they want you to cure their kidney failure. More often than not, they want to know how to manage fatigue and pain or how to have a better mood and experience less anxiety.
To address these often-overlooked symptoms, Unruh and his colleagues developed the Technology Assisted Stepped Collaborative Care trial to test whether 12 weekly sessions of cognitive behavioral therapy delivered via telemedicine could improve symptoms. They had a comparison group of patients receive weekly health education via telemedicine.
Unruh worked as the senior author alongside lead author Manisha Jhamb, M.D., M.P.H., associate professor in the Pittsburgh School of Medicine’s Renal-Electrolyte Division, to recruit a diverse pool of 160 trial participants from New Mexico and Pennsylvania who were receiving dialysis and had clinically significant levels of fatigue, pain and/or depression. Demographically, the trial group averaged 58 years in age; 28% were Black, 18% Hispanic and 13% American Indian.
“It was really exciting to have a representative sample of patients,” Unruh said. “We had patients that looked like all New Mexicans.”
The intervention was designed in a way that allowed patients to set goals and tailor the care to address their specific concerns. For example, if the patient is concerned about pain, they can focus on psychotherapies to manage that pain.
Patients were offered cognitive behavioral therapy or medication to manage depressive symptoms. Unruh said a surprising 97% of patients opted for therapy rather than medication.
“These folks on dialysis are taking a lot of medications already, so the option of getting treatment outside of medication was more attractive,” he said. “The therapy was tailored for each patient to address the unique challenges they face.”
Compared to those who received educational materials, patients who received Technology Assisted Stepped Collaborative Care had a 6% improvement in energy levels and a 10% improvement in pain severity, both of which were sustained for six months following therapy.
“It was pretty exciting,” Unruh said. “In general, having something like this that you can offer patients that’s stepped and collaborative just makes a lot of sense.” A stepped wedge trial is one in which interventions are introduced on a staggered timetable.
Unruh said that while the study’s use of telehealth was chosen to permit participation of rural New Mexicans, it proved fortunate, as the study was able to continue through the COVID-19 pandemic.
“It was serendipitous, really,” Unruh said. “In doing this, we helped ourselves manage the COVID-19 era and were able to continue this study throughout the pandemic.”
Additional authors on this research are Jennifer L. Steel, PhD; Jonathan G. Yabes, PhD; Susan M. Devaraj, PhD; Yoram Vodovotz, PhD; Scott Beach, PhD; Steven D. Weisbord, MD, M.Sc; and Bruce Rollman, MD, MPH; all of Pitt; Maria-Eleni Roumelioti, MD and Sarah Erickson, PhD, both of the University of New Mexico; and Kevin E. Vowles, PhD, of the University of Belfast in the United Kingdom.
This research was supported by the National Institutes of Health grant R01DK114085.