Preparing for Disaster: UNM Hospital Participates in Region-Wide Emergency Training
Extending the PPE Supply
UNM Health Sciences Team Devises Method to Clean and Reuse N95 Face Masks
The acronym PPE, or personal protective equipment, has been thrown around a lot lately, especially when referring to the limited numbers of N95 respirators needed to protect health care workers on the COVID-19 frontline.
With hospitals desperate to find alternatives to dwindling supplies of single-use PPE, some wondered whether used PPE could be salvaged instead of thrown away.
University of New Mexico Health Sciences Center scientists and clinical staff have joined other universities, hospitals and companies around the country in adapting a common sterilization technique to alleviate the dwindling stockpiles.
The process starts with a device made by Bioquell that is normally used to treat lab equipment with hydrogen peroxide vapor to destroy any leftover pathogens.
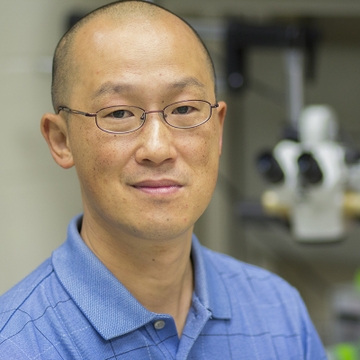
"The vapor condenses on the surface of the things you want to decontaminate, and as long as you achieve the plateau with the humidity and the concentration, then you're pretty much good to go," explains Terry Wu, PhD, associate professor in the Department of Internal Medicine.
Wu, a member of UNM's Center for Infectious Disease and Immunity, studies infectious respiratory microbes in the HSC's Biosafety Level-3 select agent laboratory and regularly uses Bioquell technology to decontaminate his equipment.
The process of adapting the technology to reprocess PPE was started by Douglas J. Perkins, PhD, professor in the Department of Internal Medicine, who began looking into how to extend the PPE supply chain in late February.
"It was becoming apparent that each place that was hit by the virus had serious shortages, because people didn't have stockpiles built up and the supply chain wasn't able to meet the demands," says Perkins, who is the director of UNM's Center for Global Health.
After searching the medical literature, one technique stood out: an HPV method developed by Battelle Memorial Institute and already in use by Battelle and Duke University, he says.
"That set the foundation for having the requisite parts in place," Perkins says. The criteria were that a mask's integrity must be maintained with multiple decontamination processes, and the disinfection method must work for up to 50 cycles per mask.
Next, the team needed to set this process up at UNM Hospitals, which was trickier than it sounds. After the process failed initially in a regular hospital room, Perkins and a team from UNMH decided to move their experiment to a vacant operating room.
This is when Wu entered the picture.
"The really nice thing about that operating room environment is it's a predesigned structure that is really ideal in many ways for decontamination with hydrogen peroxide vapor," explains Perkins. Operating rooms are sealed well, undergo many air exchanges per hour and have robust environmental controls, he says.
Wu agrees, adding that it's a lot like his own lab. And this time it worked.
Now, used masks are examined (the soiled or damaged ones are thrown away), then decontaminated with hydrogen peroxide. With each load, several biological indicators - cards coated with Geobacillus stearothermophilus bacteria spores - are stashed in the PPE racks to monitor kill efficiency.
Because these spores are more resistant to hydrogen peroxide and heat than the coronavirus, if the spores are killed it is a good measure of whether this process will work against the virus, Perkins says.
The decontaminated masks are reexamined and given to hospital workers to check for fit and then use.
With five to six racks full of N95 masks and protective eyewear, about 3,000 masks can be decontaminated per day, and they can be reprocessed up to 20 times. The masks that have already been decontaminated using this method are being used by UNMH staff.
The UNM team recently published an account of the process on medRxiv, an online resource for medical research that is awaiting peer review.
Wu says he has been working with the decontamination staff almost every day. "We're happy to help," he says. "It's a technology that we use all the time because of our research on vaccines and therapeutics against biothreat pathogens."
Perkins is excited that their protocol can be adapted to available space in any hospital using standard equipment.
"First and foremost, we wanted to get a local solution that we needed, and then not to just apply that to one environment, but rather disseminate this widely to give people some creative options to keep their health care workers safe," he says.