Telemedicine Consults Keep Patients in their Hometowns
She doesn't recall the telemedicine consult so much as the feeling of calm that it provided for her.
"Having a neurosurgeon there, being able to speak with him, gave me the confidence I needed to make decisions," she says, asking that her name be withheld.
Her husband had been found unconscious, and brought to a Roswell hospital emergency room. In the past, that would most likely have been the start of an expensive air journey to Albuquerque for evaluation by the neurosurgeons at University of New Mexico Hospital (UNMH).
But that would have been before her local hospital elected to participate in the Access to Critical Cerebral Emergency Support Services (Project ACCESS), the telemedicine consulting service provided through UNMH.
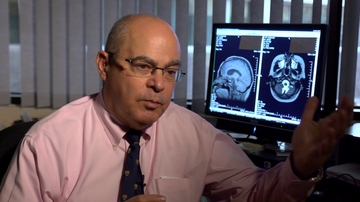
In this case, the news was not good. Neurosurgeon Howard Yonas, MD, the director of Project ACCESS, told the woman that her husband had suffered a non-recoverable stroke.
"As soon as I heard that, I knew exactly what to do," she says. "My husband had a living will and we had spoken about this before. I knew he wanted to be taken off of life of support in the event something like that ever happened."
Stroke is the fifth leading cause of death - and the leading cause of disability - for Americans, according to the U.S. Centers for Disease Control and Prevention, and it is one of the few diseases that are time- sensitive.
The most effective treatment options can vary, depending on a number of factors. In the past, RURAL hospital personnel often opted for transporting a patient to Albuquerque so that experts could evaluate a patient. Now, they can have a UNM-based neurosurgeon evaluate the patient as part of the ACCESS statewide telemedicine program. The surgeon can then explain to family members what is happening.
Project ACCESS was launched in 2015 with a three-year $15.2 million federal grant. It continues following the grant to provide rural hospitals across the state with ER-based special cameras and audio-visual conferencing with UNM neurosurgeons on a 24/7 basis.
ACCESS currently provides state-of-the-art neurology and neurosurgery expertise to rural areas, which has made it possible for many more patients to receive the best of care in their home communities. By avoiding transfers, the local hospital and community gains, and the system avoids very expensive air transports that are a major expense to the health care system.
"We now have rural hospitals who are experiencing the same success rates as stroke patients receive at an academic medical center," Yonas says.
The system has also spared many families some needless suffering.
In the past, a significant number of patients who were transferred were not suffering from a major ischemic stroke, and many could have been well treated in their hometowns. For others with catastrophic damage, the transport process placed an undue burden on family members, Yonas says.
Rather than interacting with an impersonal "robotic" machine, the ACCESS technology enables family members to speak with a neurosurgeon via a telehealth network. They can see the surgeon without having to make a long trip into Albuquerque and ask the questions they need to ask in order to make informed decisions.
"Just as visual cues are critical for a suspected stroke patient evaluation, they are also needed for conversations with a family," Yonas says. "I now can take family aside with our video conferencing service and explain the futility of any intervention and that the patient should be allowed to pass away in his community with the family at his side."
"To date, the program has performed more than 5,800 neuro-emergent consults with physicians and hospitals throughout the state," Yonas says.
Many of those consults led to a dramatic increase in the appropriate use of clot-dissolving tissue plasminogen activator (tPA,) at rural hospitals, he says. Because a neurologist can talk to the emergency room staff, patient and family using telemedicine, the appropriate use of tPA has increased from less than 2 percent to 18 percent for patients suffering from ischemic strokes.
At the same time, hospitals saw their stroke transfer rates drop by 60 percent, with a corresponding $20 million saved in air ambulance charges. All told, the ACCESS program added some $10 million to the bottom line of rural hospitals, according to Yonas.
"We want to be there for stroke patients and their families across the state," Yonas says.
"It is good to know that we can help during a difficult time without a family having to come to Albuquerque. Why make a family drive for hours in the middle of the night only to hear what they could have been told in their hometown?"