UNM Medicine
THE UNIVERSITY OF NEW MEXICO SCHOOL OF MEDICINE ALUMNI MAGAZINE
Fall 2021 edition

Cover Story: Going the Distance
New Mexico’s rural communities are scattered across more than 120,000 square miles of rugged topography, which poses problems for health care providers, especially emergency medical services (EMS).
READ
MORE
CLOSE
Cover Story: Going the Distance
EMS Consortium Celebrates 10 Years as a World-Class Program Customized for New Mexico’s Unique Needs By Paige R. Penland
New Mexico’s rural communities are scattered across more than 120,000 square miles of rugged topography, which poses problems for health care providers, especially emergency medical services (EMS).
“The primary challenge is distance,” says Darren Braude, MD, professor in the School of Medicine's Departments of Emergency Medicine and Anesthesiology & Critical Care Medicine. “That’s why we do what we do.”
Ten years ago, as Lifeguard medical director, Braude helped the university leverage its existing EMS infrastructure with the creation of the EMS Medical Direction Consortium. Today, it is a world-class model for quality community care.
The Consortium brings together university resources, such as UNM Hospital’s Level I trauma center and UNM Children’s Hospital, with a comprehensive network of New Mexico health care providers. A team of board-certified physicians with special expertise in emergency medicine forms the heart of the operation.
These faculty physicians act as medical directors for state and local agencies, such as fire rescue and police. They are available 24/7/365 by phone for providers around the state. They travel in dedicated emergency vehicles – ambulance, helicopter, or fixed-wing plane – specially outfitted with cutting-edge medical equipment and supplies.
“When we go out into the field, we may be the best-equipped life support for hundreds of miles,” says Kimberly Pruett, MD '14, assistant professor of Emergency Medicine.
This vast network of resources allows the Consortium to address health care issues strategically.
“For example, a town in Northern New Mexico just lost its ambulance service,” Pruett says. “It’s a staffing issue. In the short term, we will do lifesaving training with community stakeholders so they can keep people alive until an ambulance from a neighboring community arrives.”
“The Consortium will also play a role bringing new people into the field,” adds Joy Crook, MD, division chief of Pre-Hospital Austere and Disaster Medicine. “Like health care systems around the country, we’ve lost workers. We want to identify talented young people and get them into EMS.”
Complex problems require multifaceted solutions, which the Consortium is uniquely positioned to provide.
LIFEGUARD
Before the Consortium, there was Lifeguard. UNM Hospital began providing statewide neonatal transportation in 1975, and in 1983 expanded to provide complete emergency medical transportation as Lifeguard.
Darren Braude, MD, became Lifeguard’s medical director 20 years ago, and began expanding Lifeguard’s mission to provide rural New Mexico with some of the finest pre-hospital health care in the world. In 2011, the EMS Consortium was born.
Today, Braude is again Lifeguard Director – and at the forefront of patient transport research. “We collaborated with competing regional air companies to create standards for transporting COVID patients,” he explains. Their peer-reviewed report in the Journal of the American College of Emergency Physicians Open has been studied by EMS personnel around world.
“My mentors said, ‘I’m practicing in New Mexico, I’m doing very well, it’s great for my family, and I love it.’ This type of insight is critical when you are making long-term decisions. It is a dream come true to get the training I’ve gotten [and] to be able to practice in my home state and use my training to its maximal potential.”

BUILDING A BETTER MODEL
The Consortium combines the traditional EMS mission – reach, treat and stabilize – with a duty to expand health care access in underserved communities. Profit is not generally part of the equation.
“It’s a state entity, owned by the hospital and not for profit,” Braude says. “We have the luxury of taking two, three or four members on any ride. The University wants us to be smart and practical, but it’s mission first.”
“The traditional model is one person overseeing an EMS agency,” Crook says. “We couldn’t even provide phone coverage.” Communication goes both ways; rural health care providers are the university’s eyes and ears in the field. But they need to know that an emergency call will be answered by a highly trained physician.
“These are brilliant, dedicated medical personnel,” Pruett says. “But they appreciate having a ‘phone a friend’ option.”
While the focus is EMS, this model is agile and responsive. The Consortium evacuated the Los Alamos Medical Center during the 2011 wildfires, coordinated vaccination efforts during a hepatitis A outbreak in Bernalillo, and oversees search and rescue efforts in the Grand Canyon.
This is the team you call in when things get serious.
COMMITMENT TO COMMUNITY
To bring the University to the patient, the Consortium needed the trust and cooperation of stakeholders across New Mexico. UNM was already there.
“The university had cultivated generations of goodwill in outlying communities. It was easy to build relationships,” Pruett says. “We ask what needs they have identified, and how we can help them meet their goals.”
“Some organizations don’t ask the stakeholders, the people who live in that community, what they need,” agrees Mateo Garcia, MD '18, an EMS fellow and UNM Hospital attending physician. “UNM understands that dialogue is how we get information and build trust.”
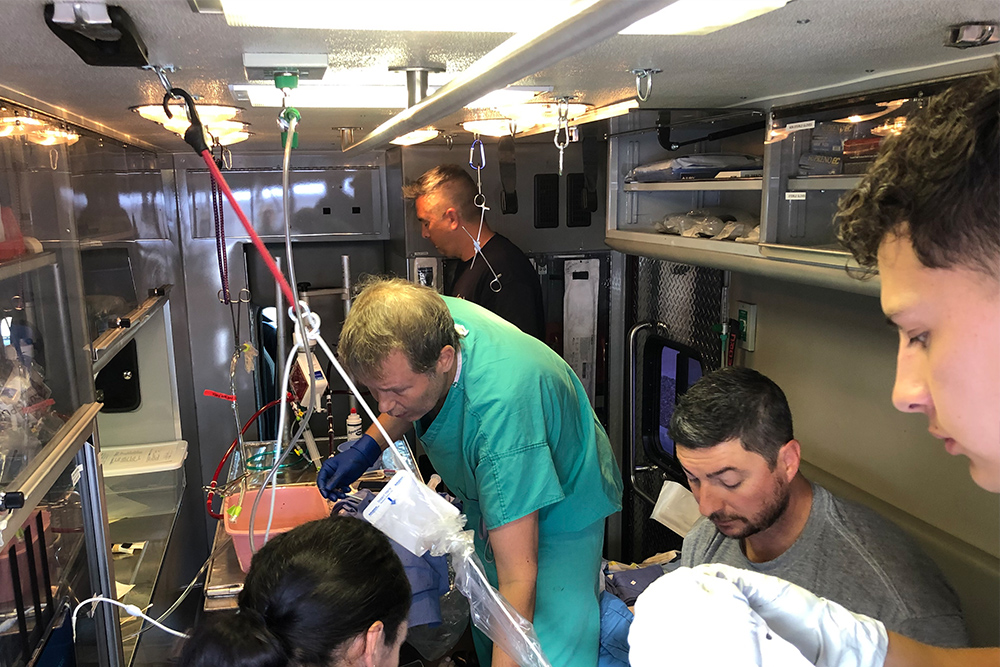
This community-centered model also allows UNMH to strategize the introduction of new technologies, such as extracorporeal membrane oxygenation (ECMO). This high-level technology can temporarily support a patient’s heart and lung function. But rural candidates in cardiac arrest can’t be transported in time. UNMH had to get that technology out into the field.
“We call it “PECMO” – pre-hospital ECMO,” says Dr. Crook. “We had to collaborate with other stakeholders, in particular Emergency Medicine leadership. And in 2019, we became the first organization in the world that could send physicians to your house and put you on an ECMO machine.”
That’s the kind of commitment to community that builds trust for another generation.

LOOKING AHEAD
The pandemic has acted as a stress test for all of New Mexico’s health care systems. The Consortium is working hard to support state and local agencies with video consultations, coordinating with regional hospitals to find open ICU beds, and of course EMS and patient transport services.
“Right now, everyone is struggling,” Garcia says. “But I want New Mexicans to know that the EMS Consortium is here help with this crisis, and the next one. You are not alone. Conscientious, thoughtful, brilliant, caring people are doing everything they can to find solutions.”


Dean's Letter
Dear alumni, colleagues, donors and friends,
I am so pleased to be representing The University of New Mexico School of Medicine as interim dean following the retirement of the remarkable Dr. Martha Cole McGrew. As we search for a new leader I wanted to share my commitment with you all to the vital and necessary projects happening at the School of Medicine.
We continue to face the COVID clinical crisis head on. Our hospital systems are running at higher volumes than ever and the amount of stress on our frontline workers is, at times, overwhelming. I want to thank all of you who provide clinical care to our patients for your willingness to keep coming back, day after day, in a tough environment. Your commitment to our patients is unmatched and unwavering.
Our diversity, equity and inclusion work continues to flourish. We are actively recruiting a diversity leader for the School and I want to thank Dr. John P. Sánchez who has worked with each department to bolster diversity efforts.
Our educational mission has weathered this COVID storm in a remarkable way. Our students are resilient, and I know that this experience will make them stronger and more capable providers. We also have had the chance to take a really deep look at ourselves.
READ
MORE
CLOSE
Dean's Letter
Dear alumni, colleagues, donors and friends,
I am so pleased to be representing The University of New Mexico School of Medicine as interim dean following the retirement of the remarkable Dr. Martha Cole McGrew. As we search for a new leader I wanted to share my commitment with you all to the vital and necessary projects happening at the School of Medicine.
We continue to face the COVID clinical crisis head on. Our hospital systems are running at higher volumes than ever and the amount of stress on our frontline workers is, at times, overwhelming. I want to thank all of you who provide clinical care to our patients for your willingness to keep coming back, day after day, in a tough environment. Your commitment to our patients is unmatched and unwavering.
Our diversity, equity and inclusion work continues to flourish. We are actively recruiting a diversity leader for the School and I want to thank Dr. John P. Sánchez who has worked with each department to bolster diversity efforts.
Our educational mission has weathered this COVID storm in a remarkable way. Our students are resilient, and I know that this experience will make them stronger and more capable providers. We also have had the chance to take a really deep look at ourselves.
Many of you may have seen our review of how clerkship grading is assessed and whether we should approach this differently. We continue to look at the data on this issue and I am proud that we are one of the first institutions to open ourselves up to this critical critique of our processes. We are committed to not only learning from this, making the changes needed but also helping teach other medical schools as they embark on this important journey.
Our more than 66 residency and fellowship programs continue to thrive at the state’s only academic health center. I am also proud to announce our full reaccreditation from the Liaison Committee on Medical Education (LCME). This is an important step to ensuring the state’s only medical school can continue to serve the people of New Mexico.
There is so much good work happening, I cannot express it all here but I hope you find this edition of UNM Medicine inspiring and that it helps you learn more about the work we continue to spearhead, here at home and across the country.
Please consider donating to the school through the UNM Foundation or to one of our scholarship programs to support our learners. You can find information on how to do that inside this magazine.
With warm regards, ![]()
Michael E. Richards, MD, MPA
Interim Dean, UNM School of Medicine
Senior Vice President for Clinical Affairs, UNM Health System
At a Glance
Ahead of the Rest | New Leadership in Education and Family & Community Medicine


At a Glance
Ahead of the Rest | New Leadership in Education and Family & Community Medicine
AHEAD OF THE REST
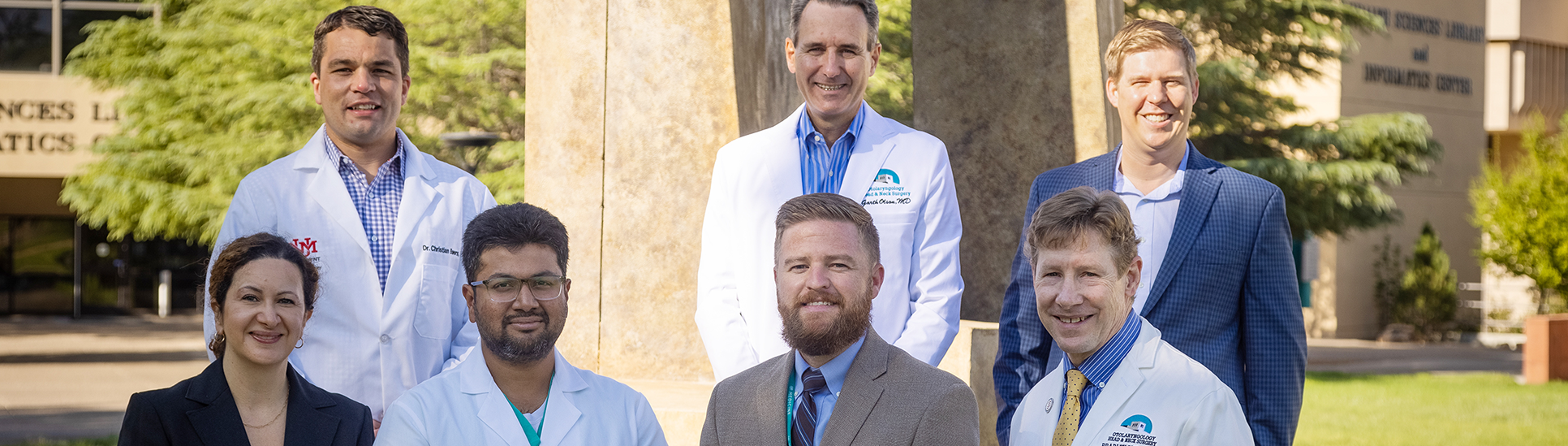
The North American Skull Base Society (NASBS) has selected The University of New Mexico School of Medicine as a Multidisciplinary Team of Distinction – one of just 28 such programs receiving the recognition.
UNM joins some prestigious programs on the 2021 list, including MD Anderson Cancer Center, Mayo Clinic, Barrow Neurological Institute and the University of Pittsburgh. It is one of just a half dozen programs located in the West.
Skull base surgery entails complex procedures in hard-to-access areas and requires the involvement of physicians from multiple specialties, said Christian Bowers, MD, vice chair for clinical affairs in the Department of Neurosurgery.
“It’s a big deal to have this recognition,” Bowers said. “We have a great team here.”
Bowers, who previously had worked at Westchester Medical Center in New York with UNM School of Medicine Neurosurgery chair Meic Schmidt, MD, completed his neurosurgery residence at the University of Utah and a skull base and cerebrovascular fellowship at Swedish Neuroscience Institute in Seattle.
He set about bolstering UNM’s skull base team when he joined the faculty in 2020. He praised colleagues in endocrinology, neuroradiology, rhinology and neuro-ophthalmology as well as his fellow neurosurgeons for their contributions. “It’s a good example of teamwork within the [School of Medicine],” he said.
Skull base surgery often involves minimally invasive procedures in which instruments are inserted through the nose or ear to access pituitary tumors, acoustical neuromas and other abnormalities.
These conditions are relatively rare, so New Mexicans benefit from the UNM team’s advanced expertise, Bowers said. “We probably average 70 pituitary cases a year,” he said. “We’re the only place doing pituitary cases in the state.”
SENIOR PROMOTION
Teresa Vigil, MD '99, has been named Interim Senior Associate Dean for Education at The University of New Mexico School of Medicine and assumed her new role on September 20.Vigil previously served as the assistant dean for Medical Student Affairs. In her new role, she oversees Medical Student Affairs, Undergraduate Medical Education, Admissions, the simulation program, the Office of Continuous Professional Education and the Health Professions programs.
“I really want to emphasize the importance of medical and health professions education and their role in the mission of the School of Medicine,” Vigil said. “We are here to serve the health needs of the people of New Mexico. The role of the School of Medicine is to maintain that and make sure we have providers who can fulfill that mission.”
Vigil grew up in Las Vegas, N.M. Her mother was a first-grade teacher and her father was a professor of political science at New Mexico Highlands University. She completed her undergraduate degree in biology at UNM, then went on to earn a certificate in medical laboratory science before working for several years at TriCore Reference Laboratories.
She started medical school at UNM in 1999 and completed her pediatrics residency there in 2007. Now a full professor, Vigil joined the Department of Pediatrics in 2007.
Vigil soon took on administrative responsibilities within the department. Over the years she has served as an associate program director, clerkship director and residency director. She spent seven years in her previous role in Medical Student Affairs.
She took over from longtime Senior Associate Dean Craig Timm, MD. Timm, a professor in the Division of Cardiology, will remain in the School of Medicine as a working retiree.
Vigil says she will focus on attracting more School of Medicine graduates to remain in New Mexico to practice. “We’ve done it in the past,” she says, “and we can do it again.”.
FAMILY & COMMUNITY MEDICINE
Rohan-Minjares Assumes Interim Chair Role
Felisha Rohan-Minjares, MD, was appointed interim chair of the UNM School of Medicine Department of Family & Community Medicine. She stepped in for David Rakel, MD, who accepted a position as chair of the Department of Family Medicine and Community Health at the University of Wisconsin.
Rohan-Minjares, a Gallup native who joined the School of Medicine faculty in 2008, served as assistant dean for clinical education and learning environments.
Rohan-Minjares started in her new role in June. “I was encouraged to consider the position by several residents and recent graduates of our residency program, in addition to members of our faculty," she said. "The encouragement of this newest generation of family physicians confirmed for me that it was the right time for my leadership to expand to all of our missions to best serve the people of New Mexico."
As the health system continues to navigate the COVID-19 pandemic, “The first thing was to ensure that we continue to hold a place of importance for primary care at UNM,” Rohan-Minjares said. She also wants to enable physician and physician assistant faculty, “to do the hard work of providing patient care, teaching and research, all at the same time.”
Rohan-Minjares said her commitment to address antiracism in medical education continues. And while she relinquished her student responsibilities in the School of Medicine, she plans to continue seeing patients at the UNM North Valley Clinic.
Rohan-Minjares completed her undergraduate studies at Notre Dame and then attended Stanford Medical School. She completed her family medicine residency at UNM, where she discovered a passion for teaching, and then-Executive Vice Dean, Martha Cole McGrew, MD, recruited her to develop a culturally effective care curriculum for medical students.
She recently received UNM’s 2020-2021 Outstanding Teacher of the Year award.
Rakel, nationally known for his work in integrative medicine, was a longtime University of Wisconsin faculty member before being recruited to head UNM’s department in 2016. He said the Department of Family & Community Medicine will be in good hands with Rohan-Minjares as interim chair.
“I think she is going to be just awesome,” Rakel said. “She’s a fantastic physician, communicator and educator. I’m excited she’s coming in and taking on that role.”

Enchanted by Design
Long before the first applications arrive at The University of New Mexico School of Medicine’s Family & Community Medicine (FCM) residency program each year, the department is already thinking about how to keep new physicians in New Mexico – preferably in underserved rural communities.
From selection to training to rural rotations, the residency program is designed with this goal in mind.
The system works. Since the School of Medicine began tracking data in 2011, around 65% of FCM residents have stayed in-state, a quarter in rural practice.
Last year, those numbers increased dramatically.
READ
MORE
CLOSE
Enchanted by Design
Family & Community Medicine Residency Retains Record Number of Physicians for New Mexico By Paige R. Penland
Long before the first applications arrive at The University of New Mexico School of Medicine’s Family & Community Medicine (FCM) residency program each year, the department is already thinking about how to keep new physicians in New Mexico – preferably in underserved rural communities.
From selection to training to rural rotations, the residency program is designed with this goal in mind.
The system works. Since the School of Medicine began tracking data in 2011, around 65% of FCM residents have stayed in-state, a quarter in rural practice.
Last year, those numbers increased dramatically.
“In 2020, an incredibly intense, difficult, heart-wrenching year for everyone in health care, 13 out of 15 residents – 87% – stayed in New Mexico, while 62% went rural,” says FCM residency director Molly McClain, MD, MPH.
“It was unusual that such a high percentage of our residents stayed,” agrees Felisha Rohan-Minjares, MD, interim chair of FCM. “It’s an interesting but intentional phenomenon.”
The intent is clear.
“UNM is a public trust,” says Arthur Kaufman, MD, Vice Chancellor for Community Health and a former FCM chair. “Our mandate is to improve state health care. This may be the most incredible outcome to date for our residency.”
The residency program uses several strategies to keep trained physicians in state, such as cultivating applicants who are from New Mexico and are more likely to practice close to home.
But in 2020, FCM graduated more out-of-state residents than normal. Yet, after a grueling year of fighting COVID in some of the country’s most remote and hardest-hit regions, almost all chose to stay.
SELECTING FOR SUCCESS
In some ways, UNM’s focus on public health inspires applicants to self-select for socially minded residents.
“We are the Department of Family and Community,” Rohan-Minjares emphasizes. “For decades UNM has recognized that caring for families, situated in communities, is the most effective way to think about the work. This connects to our residency program.”
In a normal year, FCM will review 850 applicants, interview 140, and finally choose 14 new residents. The three most important criteria that predict who will stay and serve are whether they grew up in New Mexico, whether they were educated here and whether they come from an underserved community.
According to the data, about half of all residents who meet one of these criteria will stay in-state and go into rural medicine.
“We are diligent about communicating to our own students, who are born and raised in New Mexico, who came up through our school systems, that we want them to stay at our program,” Rohan-Minjares says.
Most residents come from out-of-state, however. So, the department looks for applicants who are otherwise invested.
“We ask interviewees what they know about New Mexico, why they want to come to here,” McClain says. “We look for applicants who say that they want to live in New Mexico or practice rural medicine.”
Once all 14 residents have been selected to fulfill the University’s core mission to serve, training begins. At UNM, that means rotations into underserved communities.
RURAL EXPOSURE
“It’s about the degree of exposure, but even just one month can do it,” Kaufman says. “These towns are so welcoming. Many residents are so entranced from just a few rotations that they decide to stay.”
Some 70% of residents go on to practice within 100 miles of where they finished their residency. The department does everything it can to enhance rural experiences and improve those numbers. “We want to help residents stay in the community,” McClain says.
UNM partners with several rural residency programs in the state to expose students to underserved communities, including Gallup (pop. 21,115), Santa Rosa (pop. 2,509), and Silver City (pop. 9,162). Santa Fe (pop. 85,000) is home to one of the oldest, most successful residency programs.
“We provide training opportunities so people feel confident,” Rohan-Minjares says. “They do work in rural settings that they wouldn’t have done here at UNM Hospital, where we have so many specialists.”
“One reason why so many residents stayed in New Mexico was because of the robust experiences in rural rotations,” agrees Darshan Patel, MD, a 2020 graduate of the FCM residency now practicing in Lovington, N.M., (pop. 11,009). “That prepared us.”
Residents from big cities are also surprised by how much support small towns cheerfully provide. “In rural areas, we have a lot of community assets,” Kaufman says. “People come together. There is a lot of innovation.
The newest residency is at the Northern Navajo Medical Center in Shiprock, N.M., (pop. 7,592), which may be the first such program at an Indian Health Services facility. Modeled on the Santa Fe program, residents will spend one year in Albuquerque and two in Shiprock.
“It’s important to mention that the program was spearheaded by the faculty at Shiprock, in collaboration with UNM,” Rohan-Minjares says.
Small communities, along with the New Mexico Legislature, support the distributed rural residency program in many ways, because they know health care professionals trained in their small towns are more likely to stay there.

Join Us in Celebrating 50 Years!
 CELEBRATE BY MAKING A DIFFERENCE
CELEBRATE BY MAKING A DIFFERENCE
Support from generous donors like you allows FCM to establish fellowship programs, retain top-ranked faculty and provide educational opportunities for disadvantaged students.
With your donation, we specifically provide excellent clinical practice and specialty training, residency training, support research and educational endeavors by our faculty, and fund continuing medical education.
READ
MORE
CLOSE
Join Us in Celebrating 50 Years!
UNM School of Medicine Department of Family & Community Medicine
 CELEBRATE BY MAKING A DIFFERENCE
CELEBRATE BY MAKING A DIFFERENCE
Support from generous donors like you allows FCM to establish fellowship programs, retain top-ranked faculty and provide educational opportunities for disadvantaged students.
With your donation, we specifically provide excellent clinical practice and specialty training, residency training, support research and educational endeavors by our faculty, and fund continuing medical education.
We appreciate monetary gifts of all sizes, which will go towards current priority areas.
Priority Areas Include:
- The Warren & Rosalee Heffron Faculty & Graduate Fellowship for International Health
- Educational programs, particularly interdisciplinary training of rural primary care physicians
- Attracting and retaining dedicated minority and Native American students and residents
- Attracting and retaining dedicated, diverse, high quality faculty
- Faculty chairs and professorships
- Chair discretionary support for our department’s innovative programs
- Physician Assistant Program
Designated Gifts can be Established with the Following Contributions
Scholarship: $25,000 | Fellowship: $100,000 | Professorship: $500,000 | Chair: $1,500,000+
Let us know if you have questions about where your dollars go, or want to allocate funds to special projects or particular programs. We would like to embark on many other initiatives and hope you'll consider giving.
If you would like to make a donation, please give online at: goto.unm.edu/fcmgive.
For more information, please contact Betsy Smith at 505.313.7623 or betsy.smith@unmfund.org
To Train a Scientist
The Undergraduate Pipeline Network summer research experience seeks to cultivate students' interest in research while helping them attain skills needed to apply for and succeed in post-baccalaureate education.
The 10-week summer program, which provides the opportunity for students to choose from several areas of research, recently expanded its cancer research offerings thanks to a grant from the American Cancer Society.
READ
MORE
CLOSE
To Train a Scientist
UNDERGRADUATE PIPELINE NETWORK EXPOSES STUDENTS TO CAREERS IN RESEARCH by Michele Sequeria
The Undergraduate Pipeline Network summer research experience seeks to cultivate students' interest in research while helping them attain skills needed to apply for and succeed in post-baccalaureate education.
The 10-week summer program, which provides the opportunity for students to choose from several areas of research, recently expanded its cancer research offerings thanks to a grant from the American Cancer Society.
Students study a range of fields within the biomedical sciences. In its 11 years, the program has gone from two applicants to 160. According to Gillette, more than 95% of the students who complete the program obtain a college degree and more than half continue with further education.
No single grant supports UPN. To keep the program running, Gillette partners with several other faculty members to use grants from the UNM Comprehensive Cancer Center, the New Mexico IDeA Networks of Biomedical Research Excellence program, the UNM School of Medicine, the UNM College of Pharmacy and other sources.
"The overall goal of UPN is really to just get students excited about the health professions." - Jennifer Gillette, PhD
Most recently, a $22,000 Diversity in Cancer Research grant from the American Cancer Society awarded to Michelle Ozbun, PhD through the UNM Comprehensive Cancer Center will enable UPN to add four more students, introducing more underrepresented minority undergraduate students to cancer research.
Ozbun, a professor in the School of Medicine's Department of Molecular Genetics & Microbiology, had previously been awarded an Institutional Research Grant from the American Cancer Society, which is used to help junior faculty establish their research careers.
Now she and Gillette will extend the undergraduate program by introducing four more students to topics in cancer research and by having mentors meet with the students to advise and encourage them throughout the subsequent school year.
“The mentors would follow up with a student to see if they’re facing any barriers, doing research at their university, or thinking about applying for graduate school,” Ozbun says.
Gillette says that many students who are interested in science gravitate towards becoming a doctor because that’s a profession — sometimes the only profession — they have heard about in the biomedical sciences. Ozbun adds that some young women believe they can’t become doctors or scientists because they’re female.
“It’s exposure,” Gillette explains. “Our goal for the Undergraduate Pipeline Network is to open doors and get students thinking about what other opportunities are out there.”
If you would like to help promising students explore the possibilities of a career in research, please visit our giving page.
Brain Cancer: Hunting What's Left
Sara G.M Piccirillo studies how brain cancer makes its way back
READ
MORE
Like a mystery detective, Sara G.M. Piccirillo, PhD, is hunting deadly bad actors by studying the crime scene and questioning bystanders one by one.


Brain Cancer: Hunting What's Left
Sara G.M Piccirillo studies how brain cancer makes its way back By Michele W. Sequeira
CLOSE
Like a mystery detective, Sara G.M. Piccirillo, PhD, is hunting deadly bad actors by studying the crime scene and questioning bystanders one by one.
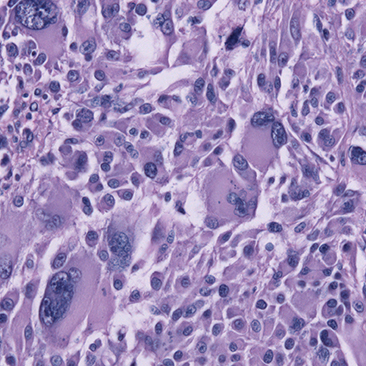
But because the bad actors she’s after are brain cancer cells – and because the bystanders are also cells in the brain – Piccirillo must use scientific methods, not police methods, to stop them in their tracks.
Piccirillo plans to use two grants, a $250,000 grant from the American Association for Cancer Research (AACR) and Novocure and a $600,000 grant from the Ben and Catherine Ivy Foundation, to study tumor cells and cells in the surrounding area, one by one.
“Glioblastoma is very heterogeneous,” Piccirillo explains. “It is not a single disease. It’s a collection of diseases that ultimately end up looking very similar.”
Even within the same tumor, the cells can differ vastly from each other, and these differences are exactly why she thinks the tumors are prone to recurring and what makes them so difficult to fight.
“They will be very heterogeneous in response to treatment,” she says.
Using the two grants, Piccirillo is focusing on residual disease, the cells that are left behind after surgery and survive treatment with chemotherapy and radiation therapy. Doctors cannot know how these cells will behave; some may seed new, aggressive tumors that resist further treatment.
“What is left behind is not equal to what is taken out,” Piccirillo says, so she is developing new ways to search for and treat these residual cancer cells.
To get a sampling of residual tumor cells, Piccirillo previously adapted a fluorescent technology that helps neurosurgeons to find and remove as much tumor as possible during brain surgery. Given as a drink before surgery, the fluorescent molecule is taken in by tumor cells, allowing the neurosurgeon to distinguish tumor from healthy cells.
In previous studies, Piccirillo’s team learned that in 65% of people with glioblastoma, tumor cells reside in a specific brain structure located outside the surgically removed tumor. Using the AACR grant, she and her team will study how cells in this structure behave before and after treatment with chemotherapy, radiation therapy and a new treatment called electric field therapy.
People with brain cancer who are treated with electric field therapy wear a cap studded with electrodes that create an alternating electric field across the brain, which has been shown in clinical studies to markedly slow brain tumor growth.
Piccirillo will use a device to mimic the electric field on individual cells. And she’s planning to conduct genomic and bioinformatics studies on the cells to learn how their behavior changes. She says, “By using genomic studies, we found that this specific area is responsible for the tumor coming back.”
Piccirillo will use the Ivy Foundation grant to study healthy cells called macrophages in the same area.
Macrophages are immune cells, but they don’t normally live in the brain, which has its own security force of immune cells called microglia. Macrophages can enter the brain and play a key role in inflammation.
“Those macrophages have at least two different identities,” says Piccirillo. “They can try to fight the tumor. Or, unfortunately, they can help the tumor to grow.”
Again, using genomic and bioinformatics analysis, Piccirillo will study macrophages and microglia from the area surrounding the tumor to discover whether they help or hinder its growth. She is excited by the newer technologies available at UNM that allow her to conduct this precise cellular analysis. “We didn’t have the opportunity before to dissect a tumor at the single-cell level,”
she says.
Sara G.M. Piccirillo, PhD, is The Robert M. Faxon Jr. Endowed Professor in Neuro-Oncology; assistant professor in the UNM School of Medicine Department of Cell Biology & Physiology, and holds a secondary appointment in the Department of Neurosurgery. She is a full member of the Cellular and Molecular Oncology Research Group at the UNM Comprehensive Cancer Center.
Dr. Piccirillo’s research team includes:
- Christian Bowers, MD, associate professor and vice chair of Clinical Affairs, Department of Neurosurgery, UNM School of Medicine
- Scott Ness, PhD, Victor and Ruby Hansen Surface Endowed Professor in Cancer Genomics; professor, Department of Internal Medicine, Division of Molecular Medicine, UNM School of Medicine; associate director, Shared Resources and director, Analytical and Translational Genomics Shared Resource, UNM Comprehensive Cancer Center
- Yan Guo, PhD, associate professor, Department of Internal Medicine Division of Molecular Medicine, UNM School of Medicine; director. Bioinformatics Shared Resource, UNM Comprehensive Cancer Center.

Student Affairs: A Lasting Impression
When I was a child, dental hygiene and routine visits were not a priority.
I grew up in a low-income family and only had access to a community clinic for my dental needs. The lack of care came with dental issues, such as cavities and crooked teeth. I had to improve my dental health, especially if I wanted to fix the crowding.
I went to see a dental hygienist, who provided excellent care and tailored a treatment plan according to my needs. She never made me feel bad about my teeth – she educated me on how I could do better and stressed the importance of my dental health in and out of the office.
READ
MORE

CLOSE
Student Affairs: A Lasting Impression
by Tenisha Marquez - B.S. Dental Hygiene class of 2022
When I was a child, dental hygiene and routine visits were not a priority.
I grew up in a low-income family and only had access to a community clinic for my dental needs. The lack of care came with dental issues, such as cavities and crooked teeth. I had to improve my dental health, especially if I wanted to fix the crowding.
I went to see a dental hygienist, who provided excellent care and tailored a treatment plan according to my needs. She never made me feel bad about my teeth – she educated me on how I could do better and stressed the importance of my dental health in and out of the office.
All that it took for me to understand the importance of dental hygiene was someone taking the time to sympathize with my circumstances and give me the information and care I needed. Now that I had proper dental health, I was able to see an orthodontist at another community clinic. He was very professional and involved with his patients.
I once remarked that I wanted to pursue a career in the dental field, and any time I would visit he made sure to encourage my dream. My time with the dental hygienist and orthodontist affirmed my desire to help others by becoming a part of the dental field.
I decided to pursue dental assisting to get my foot in the door of the dentistry. I have been a dental assistant for the past 10 years and have loved every minute of it. I was also fortunate enough to further my education and go back to school for dental hygiene.
I am grateful and privileged to be a senior in the Dental Hygiene program at The University of New Mexico. Helping my patients achieve a better and healthier smile through education and care is my purpose, but my dental background is only a portion of why I love my career.
Beyond dentistry, building a trusting and long-lasting relationship with my patients is truly my “why.” The past three years have not been the easiest, with juggling my roles as a wife, mother of two amazing children, and a student. Despite the challenges, I know it is well worth it.
I am excited to graduate in the spring of 2022 and live out my dreams as a dental hygienist.

Dental Health for New Mexico and Beyond
DIVISION OF DENTAL HYGIENE, DEPARTMENT OF DENTAL MEDICINE
READ
MORE
Known nationwide for its focus on dental public health education and developing dental providers to treat those who are underserved, the School of Medicine is proud to be home to the Department of Dental Medicine's Division of Dental Hygiene.

Dental Health for New Mexico and Beyond
DIVISION OF DENTAL HYGIENE, DEPARTMENT OF DENTAL MEDICINE
CLOSE
Known nationwide for its focus on dental public health education and developing dental providers to treat those who are underserved, the School of Medicine is proud to be home to the Department of Dental Medicine's Division of Dental Hygiene.
The Divison educates future dental hygienists through its bachelor of science in dental hygiene, bachelor of science in dental hygiene degree completion and master of science in dental health programs. These programs increase UNM’s reach and ability to transform the practice.
The master of science in dental health was the first graduate dental hygiene program west of the Mississippi. Students are trained to develop programs, conduct research and educate the public on the need for routine preventive dental care. Alumni have been spotlighted on the national stage for their efforts to advance dental hygiene science and practice.
Currently in development is a PhD in dental hygiene program, which will focus on dental hygiene research. It will be the first dental hygiene doctoral program in the nation.
The Division has been instrumental in educating dental hygiene faculty across the country on teaching strategies to truly transform dental hygiene care for the past 20 years.
Thousands of dental hygiene faculty have taken part in workshops that have focused on educating providers who will be providing direct access to dental hygiene integrated into primary care systems, hospitals and schools.
Dental Hygiene faculty are leaders in dental hygiene nationwide. They serve in various offices with dental hygiene associations, conduct the research and write the textbooks used in this transformation.

Chasing Trains
Have you ever had the feeling?
You are tripping down the stairs to catch the rush hour train. Sand crunches under your warm Friday afternoon sneakers as you navigate the bottom steps, weaving around the casually placed hipster undoubtedly standing in your path. The city is boiling with potential, and you are feeling it churn through you on this mad evening dash.
You could have left work just a few minutes earlier; a more responsible, less dramatic version of yourself would have. Yet, some part of you, after hours of clicking and clacking at your desk, yearned for the chase. The truth was you knew exactly what you were doing as you watched the time pass by on the corner of your screen.
READ
MORE
CLOSE
Chasing Trains
By Supreetha Gubbala, MD | PGY III Family Medicine Resident
Have you ever had the feeling?
You are tripping down the stairs to catch the rush hour train. Sand crunches under your warm Friday afternoon sneakers as you navigate the bottom steps, weaving around the casually placed hipster undoubtedly standing in your path. The city is boiling with potential, and you are feeling it churn through you on this mad evening dash.
You could have left work just a few minutes earlier; a more responsible, less dramatic version of yourself would have. Yet, some part of you, after hours of clicking and clacking at your desk, yearned for the chase. The truth was you knew exactly what you were doing as you watched the time pass by on the corner of your screen.
It is incredible how liberating 30 seconds of sprinting for a completely unimportant train can be. For those few seconds, you were not who you were at 5 p.m. on a Friday afternoon. You were, instead, what you were running toward. Maybe you hadn’t exercised in four months, but somehow your legs were moving. You could barely complete your stack of clinic notes, yet your mind was analyzing the shortest distance between the steps and the train door. Each cell in your body moved toward a single purpose and the burning in your chest reminded you what it’s like to be at the edge of yourself.
I turned 30 during the peak of the greatest infectious pandemic the world had witnessed since the Spanish flu. My bets had always been placed on a more thrilling version of the apocalypse, filled with star-crossed love, betrayal and possibly, crossbows. What I did not expect was how harrowingly mind-numbing it would be.
Whether or not I like it, I am a family medicine resident and this pandemic is the bedmate I never chose. It is what I wake up to, what I eat dinner reading about and what I fall asleep praying for. Even against this backdrop the privilege of my profession allows me to constantly be rushing between witnessing the birth of new life, the flickering of death and always, too many unjust deaths.
Yet, I recently found myself staring at a cage in Petco, watching a hamster run on a red plastic wheel. I felt oddly connected to its beady black eyes peering straight ahead, putting one foot in front of another with seeming purpose, but heading nowhere in particular. I remembered the discomfort I felt every time I walked by the “Heroes Work Here,” signs at the hospital entrance. Why did chasing subway trains during medical school feel so much more purposeful than the life and death I witnessed every day?
I came to realize turning 30 during a global pandemic came with many gifts the previous decade of my life could not afford me. Self-acceptance and peace with my limitations arrived as hard-earned lessons of survival this year. They became essential to not being consumed by the increasingly complex microcosm of serving a human being in a hospital bed.
However, somehow in my dance of embracing things as they were, I lost my ability to chase trains. The pandemic that had made me face the fragility of life while turning 30 had made me comfortable with contentment and safety. Spontaneity, risk, and therefore, true vulnerability now felt like faded photographs, falling out of forgotten journals on the pulpit of a stranger who no longer lived in my home.
Recently, I went back to my hometown of Boston. Visions of that fearless twenty-something-year-old woman with her black leather boots flooded my memory as I trotted along the South Boston streets and bars that raised her. As I approached the commuter rail entrance of Back Bay station, I smiled at the familiar orange Creamsicle sign I had rushed past so many times before. While reminiscing, my eyes drifted to my outbound train time: “ARRIVING” shone in bright capital letters.
It was time. Maybe it was the nostalgia, or the nearly five pounds of dim sum I had consumed that morning in Chinatown, but my legs flew. My chest burned, as my mind swarmed with visions of apoplectic zombies, strangely donning grungy stethoscopes. I shook my head and focused on the long stairwell ahead.
For a moment, I wasn’t sure who I was running from, or whether the mind-numbed partially human figures of my imagination were simply versions of myself. I slid through the closing doors and the surprised conductor smirked at me with a little Bostonian pride:
“Well, looks like you made it, kid.” His accent felt like honey on my hardened heart, and the word “kid” inevitably made me chuckle. My heart still pounding, wary of the breathless gasping coming out of my mouth, I sat down and suddenly began to laugh.
The deep rumble of laughter was an eruption of a deep forgotten joy. What it felt like to not be careful, to leap into an unknown outcome and throw all of yourself in anyways.
Something changed in me when this pandemic hit and I simultaneously left my twenties. Life became so coveted that I stopped taking risks and started instead running along a double-edged sword of acceptance, dipping into numbing complacency because it was safer than what was happening in hospital beds around me.
I could call it burnout, but it feels like a much larger reckoning with myself than just the overworked loss of my humanity. It felt like the only form of survival I could choose at the time, and maybe I am finally starting to choose differently.
Someone recently sent me a comic entitled, “No one is OK right now.” I laughed, because I could not help but be impressed by how accurate that statement is. No one is really OK. We have all found a new version of normal in this strange year sitting in our rearview mirrors, but we have to reckon with how it may have deeply changed the people we once were. For some of us that means severe anxiety, and for others, it can be a comfortable numbing.
I know I am not the only zombie physician human, thawing out the soul that brought them to this work. Sadly, I have started to find more of us, in lingering glances and silent moments of conversation in hospital work rooms.
This year, I have lost touch with that girl who runs full speed toward the unknown, messy bun flailing and boots clacking towards an outcome that is far from guaranteed. Maybe it is not too late for me to catch that last train across a packed subway platform; to dare to step off the hamster wheel of survival to live in the unknown fragility of life while experiencing the beautiful wholeness that comes with vulnerability.
Crossbows and star-cross zombie love stories might have to wait a little bit longer.

Social & Emotional Connection
Supporting our Internal Medicine House Staff
Prism Fund for Physician Well-Being
In order to respond to the added pressures of the pandemic on Internal Medicine house staff, please help the Office of Professional Well-being and the Internal Medicine Residency at the UNM School of Medicine provide opportunities to enhance social and emotional connection among trainees.
READ
MORE
CLOSE
Support our Trainees
Supporting our Internal Medicine House Staff
Prism Fund for Physician Well-Being
In order to respond to the added pressures of the pandemic on Internal Medicine house staff, please help the Office of Professional Well-being and the Internal Medicine Residency at the UNM School of Medicine provide opportunities to enhance social and emotional connection among trainees.
These connections, which normally would happen organically, have been hindered because of added workload and idolation brought on by the pandemic.
TO DONATE, PLEASE CLICK HERE.
Giving by the Numbers

in scholarships awarded

total gifts & pledges

unique donors

total # of gifts

in endowment gifts

current total endowments

new bequests

est. total value of bequests

in gifts to the dean's fund

Giving Profile
“I have to get a picture of that.”
It had been this way for days - cellphone snapshots of the routine walk around the neighborhood with Layla, a Chihuahua Terrier mix and Dr. Martha Cole McGrew’s cherished companion, a selfie with faculty leaders and social posts with students and learners grabbing her for one more goodbye.
McGrew wanted to remember it all. After all, The University of New Mexico School of Medicine has set the scene for the past 31 years of her life and career. In September of this year, she retired from the School of Medicine to start her next chapter with a new love, her first grandson.
It’s not enough to just say she spent three decades on North Campus, her work, contributions, creations and influence are immeasurable.
So where did she get her passion for service?
READ
MORE
CLOSE
Giving Profile
PASSION FOR COMPASSION: Martha Cole McGrew reflects on more than 30 years of service and giving By Ashley Salazar
“I have to get a picture of that.”
It had been this way for days - cellphone snapshots of the routine walk around the neighborhood with Layla, a Chihuahua Terrier mix and Dr. Martha Cole McGrew’s cherished companion, a selfie with faculty leaders and social posts with students and learners grabbing her for one more goodbye.
McGrew wanted to remember it all. After all, The University of New Mexico School of Medicine has set the scene for the past 31 years of her life and career. In September of this year, she retired from the School of Medicine to start her next chapter with a new love, her first grandson.
It’s not enough to just say she spent three decades on North Campus, her work, contributions, creations and influence are immeasurable.
So where did she get her passion for service?
The Coles: A Service-Minded Family
McGrew’s parents dedicated their lives to helping people who needed them most.
Her father, Dr. Shelton Cole, was a first-generation physician, who returned to his small community of Gibsland, La., in the 1960s to practice. He was the only doctor in the area and often could be found treating patients right at their kitchen table.
McGrew’s mother, Maxine, worked with him to provide care and support to the members of their community. McGrew credits her for teaching her resilience and perseverance after her father suddenly died when she was a young girl.
“My mother helped him in his office, and she would drive people to appointments, take food to people, or do things in service to the people, so they were a pair in that community,” McGrew said.
McGrew’s parents didn’t just teach what it meant to be a good member of their community, they lived it, and expected the same from their children.
“My mother always said that, "To whom much is given much is expected," and while we were relatively poor, we had more than many, so we learned to serve where there was need,”
McGrew said.
UNM: A Place to Serve
UNM School of Medicine's Department of Family and Community Medicine (FCM) proved to be the right place for McGrew to fulfill her desire to serve. Fresh from a fellowship at the University of California, San Francisco, McGrew took a faculty position under Warren Heffron, MD, and Arthur Kaufman, MD, in the FCM department. “They gave me an incredible opportunity to do things I loved – teach, practice, create and innovate,” McGrew said.
On top of teaching and patient care, McGrew was asked to support grant writing for educational and teaching opportunities.
“The first grant I wrote was to Health Resources and Services Administration in 1992, to establish a clerkship in Family Medicine,” she said.
Before that, there was no required clerkship in the department. McGrew then became the first director for the very clerkship she worked to establish. Her career in leadership took off, and she went on to hold the titles of vice chair for education, then associate chair, and in 2008, became the very first woman and first family medicine residency-trained physician to serve as the School's FCM chair. In 2015, she assumed the role of executive vice dean of the School of Medicine.
When Chancellor and Dean Paul Roth, MD, MS, retired in 2020, McGrew was appointed Interim Dean of the School of Medicine. She took the reins at the peak of the COVID crisis, something that required commitment and steady leadership.
Despite these challenges, the School earned full accreditation from Accreditation Counsel for Graduate Medical Education, all education programs continued throughout the pandemic, and she reinvigorated the School's diversity efforts.
The Future: Giving Continuity
While McGrew's physical time at UNM has come to a close, she will never step away fully from the School of Medicine and the programs she loves. She used her retirement to seek donations for the Cole Family Endowment she created in 2015. The fund provides scholarships to students who come from New Mexico counties that are medically underserved. It’s her way to honor the good work that the entire Cole family has done and will do in the future.
“It’s a good feeling to know that you may have had some little part in making it just a little bit better or easier for someone else. It’s the best feeling of accomplishment – along with delivering a baby.”
In celebration of her, the School of Medicine's department chairs established a new fund in McGrew’s name. This fund is tied to another area that she cares about deeply — diversity. The Martha Cole McGrew Faculty Award for Commitment to Education and Diversity in Medicine will be presented to an outstanding faculty member who demonstrates a long-standing commitment to advancing the mission in the areas of education and diversity.
"It is important to honor people who are doing the work that the UNM medical school was called to do, which is to create a health care workforce for New Mexico, and the goal of creating a more diverse workforce for our diverse population is critical,” McGrew said, “I want to honor people who have committed their careers to education and diversity. Those two areas are often not as recognized and rewarded as the missions of clinical care and research.”
Honor Dr. Martha Cole McGrew in her retirement by contributing to The Cole Family Scholarship or The Martha Cole McGrew Faculty Award for Commitment to Education and Diversity in Medicine through the UNM Foundation.
Give online today.

President’s Letter
Hello Lobo MDs,
The summer and fall months of 2021 brought opportunities for MD alumni to re-engage with the UNM School of Medicine community after the COVID hiatus. Social distancing produced virtual components to all of our traditional events, allowing our outreach to extend to house staff and MD alumni across the nation. As we broaden our involvement, the impact of our mission expands. Thank you to all who participated in these events. Please read on to learn more about some of our exciting accomplishments.
READ
MORE
CLOSE
President’s Letter
THE UNIVERSITY OF NEW MEXICO SCHOOL OF MEDICINE ALUMNI ASSOCIATION
Hello Lobo MDs,
The summer and fall months of 2021 brought opportunities for MD alumni to re-engage with the UNM School of Medicine community after the COVID hiatus. Social distancing produced virtual components to all of our traditional events, allowing our outreach to extend to house staff and MD alumni across the nation. As we broaden our involvement, the impact of our mission expands. Thank you to all who participated in these events. Please read on to learn more about some of our exciting accomplishments.
 LOBO MD BRANDING
LOBO MD BRANDING
Everyone’s a Lobo – Woof, Woof, Woof! Having a brand that identifies us as a proud member of the UNM community is important. Our Lobo MD moniker is a way to proudly display our appreciation and support for the UNM School of Medicine. We will have a full range of attire coming to an online store near you.
NAMED LOBO MD SCHOLARSHIPS
As you may be aware, your continued financial support created an endowment that supports annually 10 $2,500 scholarships for third- and fourth-year medical students. To reach an even greater number of our students with financial need, the Alumni Association has launched the named Lobo MD Scholarship initiative.
Give $1,000 or more to create and name a new scholarship. One hundred percent of your donation is awarded directly to a deserving medical student. To date, we have raised more than $25,000 and have high hopes to reach our $40,000 goal by the end of June 2022.
STUDENT SUPPORT
The ever-popular Nook returned to full operation this fall, providing free snacks and coffee to our learners, thanks to your generous support. The annual White Coat campaign continued its tradition of providing the first white coat to every member of each new UNM MD class. During this year's White Coat ceremony, one of our new Alumni Association board members, Jaren Trost, MD '15, spoke to the UNM MD class of 2025 about the importance of providing care here in New Mexico.
ENDURING CONNECTIONS
The Serve NM and Coming Home campaigns reached alumni near and far this summer, delivering care packages for those who have roamed beyond the Land of Enchantment, as well as those who are serving the people of New Mexico during residency. Both packages served a common purpose: to strengthen the connection between New Mexico and its UNM-trained physicians.
Enjoy the many stories of how the UNM School of Medicine – and your fellow Lobo MDs – advance the health of all New Mexicans. Please stay connected in the coming year and always show your Lobo pride.
Sincerely,
C. Nathaniel Roybal, MD, PhD ’07
President, Alumni Association
UNM School of Medicine
BOARD REPORT
UNM SCHOOL OF MEDICINE ALUMNI ASSOCIATION
BOARD OF DIRECTORS
C. Nathaniel Roybal, MD, PhD ’07 (President)
Alisha Parada, MD ’08 (Treasurer/Vice President)
Jennifer Phillips, MD ’01 (Immediate Past President)
Lawrence Andrade, MD ’00
Manuel Archuleta, MD ’73
Valerie Carrejo, MD ’04
Dion Gallant, MD ’99
Angela Gallegos-Macias, MD ’02
Albert Kwan, MD ’83
Mario Leyba, MD ’04
Athanasios Manole, MD ’14
Robert Melendez, MD ’08
Daphne Olson, MD ’17
Mario Pacheco, MD ‘86
Valerie Romero-Leggott, MD ’92
Linda Stogner, MD ’83
Jaren Trost, MD ’15
STUDENT & RESIDENT REPRESENTATIVES
Jessica K. Benally, MS ’22
Kelli Duran, MS ’23
EX-OFFICIO MEMBER
Michael E. Richards, MD, MPA
Interim Dean, UNM School of Medicine
ADVANCEMENT AND ALUMNI RELATIONS
CHIEF ADVANCEMENT AND
EXTERNAL RELATIONS OFFICER
Ashley Salazar
PROGRAM MANAGER
Erika Anderson
OPERATIONS SPECIALIST
Ashley Hatcher
EVENTS PLANNER
Ruth Morgan
OPERATIONS ASSISTANT
Cara Sego
CONTACT
UNM School of Medicine
Office of Advancement and Alumni Relations
MSC 08 4720 • Fitz Hall #182B
1 University of New Mexico
Albuquerque, NM 87131-0001
505.272.5112
2021 Alumni Reunion Snapshots




















All of our alumni are class acts.
Help us brag a little! Please send us your good news, personal or professional, to share in UNM Medicine.
Email us at unmsomalumni@salud.unm.edu or give us a call at 505.272.5112
UNM School of Medicine
Office of Advancement & Alumni Relations
READ
MORE
CLOSE
CLASS ACTS
Help us brag a little! Please send us your good news, personal or professional, to share in UNM Medicine.
Email us at unmsomalumni@salud.unm.edu or give us a call at 505.272.5112
UNM School of Medicine
Office of Advancement & Alumni Relations
Alumni
Alfredo Ramon Vigil, MD ’77
Dr. Vigil is celebrating his retirement after serving the people of Taos, over a 40-year career. Congratulations, Dr. Vigil! Thank you for serving the mission of The UNM School of Medicine by advancing the health of all New Mexicans.
Michael F. Hartshorne, MD ’78
UNM Medicine alumni are sought after as content experts in many areas. Live Science interviewed Dr. Hartshorne to help explain why and how dark shadows were left behind after an atomic bomb was detonated at Hiroshima in 1945 (www.livescience.com/nuclear-bomb-wwii-shadows.html).
Melvina McCabe, MD ’84
Dr. McCabe contributed to the creation of “Vaccination from the Misinformation Virus,” a documentary that aims to help parents and community leaders understand the importance and safety of vaccines. The film premiered in Phoenix in July and to be streamed via the School of Medicine’s YouTube channel as part of the Community Lecture Series on December 2.
Robert E. Sapién, MD ’86
The Spears School of Business at Oklahoma State University welcomed its newest class, Cohort X, to the PhD in Business for Executives program. A familiar face in Cohort X is that of School of Medicine alumnus, Dr. Robert Sapién.
Charles Pace, MD, PhD ’96
Dr. Pace was named one of the “5 Best Pain Management Doctors in Albuquerque” by Kev’s Best, an independent blog that reviews and lists their views on the best businesses and major consumer markets across the country.
Laura Parajon, MD ’95
Dr. Parajon was awarded the American Academy of Family Physicians Public Health Award in recognition of her important contributions as a family physician to advancing the health of the public at the national, state and local level. She is deputy cabinet secretary in the New Mexico Department of Health and an assistant professor in the UNM Department of Family & Community Medicine.
C. Dana Clark, MD ’03
Dr. Clark was named one of “10 Total Joint ASC Physicians to Know” by Becker’s ASC Review, a business and clinical news site run by Becker’s Healthcare. He is one of only 10 doctors mentioned from across the country.
Lana Dolores Melendres-Groves, MD ’04
Dr. Melendres-Groves served as a featured expert speaker for the National Broadcast Series through United Therapeutics and the Pulmonary Arterial Hypertension (PAH) initiative. These virtual events educated people with PAH and their caregivers, providing insights and perspectives about how to manage life with their condition.
House Staff Alumni
Matthew David Katz, MD
Dr. Katz has joined CARTI, a statewide cancer care provider in Arkansas. Congratulations on your new position, Dr. Katz.
Jeremy T. Phelps, MD
An accredited neurosurgeon with INTEGRIS Spine and Neurological, Dr. Phelps was named one of Oklahoma’s five best neurosurgeons by Kev’s Best, an independent blog that reviews and lists their views on the best businesses and major consumer markets across the country.
Catherine Tchanque-Fossuo, MD
Western Dermatology Consultants welcomed Dr. Tchanque-Fossuo as a new provider as of July 2021. Congratulations on your new position, Dr. Tchanque-Fossuo.
Thomas Bernasek, MD
Dr. Bernasek was included as one of “10 Total Joint ASC Physicians to Know” by Becker’s ASC Review, a business and clinical news site run by Becker’s Healthcare.
Robert Zuniga, MD
Dr. Zuniga was named one of Albuquerque’s “5 Best Pain Management Doctors” by Kev’s Best, an independent blog that reviews and lists their views on the best businesses and major consumer markets across the country.
Faculty
Mary Ann Osley, PhD & Douglas Ziedonis, MD, MPH
UNM recently announced the promotion and honor of 10 faculty members, including Drs. Osley and Ziedonis, to the rank of Distinguished Professor, the highest title that UNM bestows upon its faculty.
Gurdeep Singh, DO
Dr. Singh was promoted to executive diversity and well-being officer at the UNM Sandoval Regional Medical Center in Rio Rancho. Dr. Singh is also an assistant professor in the Department of Internal Medicine. The new role includes leading a comprehensive diversity, equity, inclusion and well-being strategy for SRMC, working with hospital leadership to implement proactive diversity, equity, inclusion and well-being initiatives. Congratulations, Dr. Singh.
David S. Schade, MD & R. Philip Eaton, MD
Drs. Schade and Eaton successfully partnered to spearhead efforts in the New Mexico Legislature to require insurance coverage for coronary artery calcium screening, a proven method for detecting cardiovascular disease, and the pair continues to push to expand coronary artery insurance coverage.
Gulshan Parasher, MD
In 2020, the UNM Board of Regents and the School of Medicine honored Dr. Robert Strickland by approving the creation of an endowed distinguished chair in Strickland’s name to advance digestive health and science. In October, the School of Medicine announced the naming of Dr. Parasher as the inaugural Strickland Distinguished Chair.
Ann Gateley, MD
Dr. Gateley received the 2021 Outstanding Alumna Award at Sweet Briar College. The award was created to honor alumnae for their outstanding service to Sweet Briar in a volunteer capacity. After college, Gateley attended medical school at UNM and went on to be a sports medicine specialist, team doctor for UNM Athletics Department and Internal Medicine program director.
Gerald D. Otis, PhD
Dr. Otis hosted a book signing in Las Cruces, N.M., in July. Dr. Otis has written four books: Joseph Lee Heywood: His Life and Tragic Death (2011), Paroxysm: Love, Murder and Justice in Post-Civil War Washington, D.C. (2013), Presumed Crazy: A Fisherman Gets Entangled in the Mental Health Gulag (2014) and Physician Career Choice and Satisfaction (2019). He is currently at work on a new novel inspired by his work with veterans.
William F. Rayburn, MD
Dr. Rayburn was recently highlighted in an alumni spotlight by the University of Texas at Dallas MBA program. His many accomplishments include founding the Workforce Studies and Planning Initiative at the American College of Obstetricians and Gynecologists, as well as his time as the long-standing chair of UNM’s Department of Obstetrics & Gynecology, and his multiple national leadership positions in medical education.

The University of New Mexico School of Medicine extends our sincere sympathies to the loved ones of our departed alumni and faculty.
To submit information on a departed member of our alumni or faculty, email us at unmsomalumni@salud.unm.edu or call 505.272.5112
UNM School of Medicine
Office of Advancement & Alumni Relations
READ
MORE
CLOSE
IN MEMORIAM
To submit information on a departed member of our alumni or faculty, email us at unmsomalumni@salud.unm.edu or call 505.272.5112
UNM School of Medicine
Office of Advancement & Alumni Relations
Alumni
Sergio A. De Haro, PhD ’09, died on July 2, 2021, due to complications from renal disease. His doctorate work made important contributions to the understanding of Mycobacterium tuberculosis infection of white blood cells, and his research further contributed to the understanding of the human papillomavirus, other infectious diseases and cancer. De Haro taught biochemistry at UNM and anatomy and physiology at Central New Mexico Community College. He was passionate about his students, many of whom went on to become professionals in science and health care.
Christopher Peter Allen, PhD ’03, died on May 23, 2021, in Fort Collins, Colo., from complications of pancreatic cancer treatment. His specialty was DNA and cancer research. A highlight of his scientific career was a two-year span of time featuring multiple trips to Japan, where he conducted basic cell research using carbon-ion radiation. He leaves the legacy of an operational flow cytometry core to the Colorado State University research community.
Bernard Henry “Biff" Bueffel III, MD ’70, died on January 15, 2021. He started a pediatric practice in Portland in 1976 and followed his true passion of caring for children and families for 37 years.
John Andrew "Andy" Cameron, MD ’72, died on January 7, 2021. He worked as an emergency room physician for approximately 30 years, mostly at Washoe Medical Center and Renown Health. He was also a member of the National Guard, working as a military doctor. He re-enlisted after the attacks on 9/11 and rose to the rank of colonel after serving tours in Afghanistan and Iraq.
Wayne A. Delamater, MD ’75, died on January 18, 2021. He practiced ophthalmology for almost 40 years. He loved serving his patients, and they loved him because of it. He also loved his loyal staff, many of whom were with him all the years he was in practice.
Lawrence Kano Inouye, PhD ’88, died on February 2, 2021. He worked for the Hawaii Department of Health as an epidemiological specialist until his retirement.
Lawrence Larkin, MD ’74, died on October 25, 2020, surrounded by his wife and daughters. He was a retired radiologist who practiced in Lynchburg, Va., for 25 years. He served as chief of Radiology at Eglin Air Force Base Hospital and received an honorable discharge in 1980, having achieved the rank of major. Larkin and his growing family moved to Virginia in 1980, where he joined Radiology Consultants of Lynchburg. He practiced until 2005, when he retired for medical reasons.
Thomas McGuire, MD ’83, died on June 23, 2021, a victim of respiratory failure and Huntington’s disease. McGuire practiced medicine at Independence Regional Health Center, where he directed the rehabilitation unit and a head trauma unit. For more than 25 years, he participated in the Archdiocese of Santa Fe's Pilgrimages for Vocations, which he began during a fellowship with a local physician in Taos.
Leonard Ray Ramsey, MD ’81, died on January 8, 2021. After residency, he and his family moved to Bozeman, Mont., where he worked with the Medical Associates group. In 1989, he served a three-month medical mission to Swaziland and then served four years with World Gospel Mission at Tenwek Hospital in the highlands of Kenya. Ramsey and his family founded Hope of the Nations Tanzania alongside Coni and Harold Knepper. He served the lake people, providing life-giving health care to “mamas and watoto” (children). He even learned to fly a helicopter and used it to reach people living along the lake. Ramsey returned from ministering in Africa in 2011, and retired from medicine in May 2019.
Mark David Rieb, MD, NMD ’80, died on October 20, 2020. Rieb was a family physician for 40 years in both Minnesota and New Mexico, with specializations in obstetrics, acupuncture and naturopathic medicine. He was beloved by his many patients and kept his license active after retirement, volunteering with the New Mexico Medical Reserve Corps.
House Staff Alumni
Michael Davidson, MD, PhD (Fellow – Infectious Disease), died in Anchorage, Alaska, from COVID-19 on November 8, 2020. His choice to spend much of his career studying infectious disease may well have been spurred by the death of his grandparents during the Spanish Flu pandemic. In addition to his MD, Dr. Davidson earned a master of public health degree and a PhD in epidemiology from Johns Hopkins University. He was also an affiliate professor with the biomedical program at the University of Alaska.
Raphael J. DeHoratius, MD (Fellow – Internal Medicine), passed away suddenly on November 26, 2020, at his home in Upper Gwynedd, Penn. He was a leading rheumatologist in Philadelphia, where he developed the city’s first lupus center. He served as president of the American College of Rheumatology in 2002-2003, and was awarded both the title of Master in Rheumatology and the Hollander Award. He went on to serve as medical director in rheumatology at Johnson & Johnson until his retirement in 2017.
Robert W. Benson, MD (Resident - Orthopaedic Surgery), died on November 28, 2020. He was a loving husband and father, a devoted doctor whose life work was helping others. He was also “Captain Ziggy” – a hot air balloon pilot and longtime participant in the Albuquerque International Balloon Fiesta. He was a joyful and active man whose laugh could be heard miles away.
Edwin Chappabittty, Jr., MD (Resident - Family Practice), died on June 15, 2021. He served in Vietnam in 1969 and 1970, where he received numerous awards for valor. Chappabitty was commissioned in the U.S. Public Health Service and assigned to the hospital in which he was born, the Lawton Indian Hospital in Lawton, Okla. For the next 25 years, he served as a family practice physician at hospitals in Anadarko, Okla., and Lawton, and was three-time department chairman at Lawton. In 1996, he was honored by the Association of American Indian Physicians as Physician of the Year. He received the Hero Award in the Journal of Minority Medical Students in 1997. After retiring in 2008, he went on to serve as the first medical director of the Comanche Nation in Lawton.
Basia Holub, MD (Resident - Emergency Medicine), died unexpectedly on March 29, 2021. Dr. Holub embarked on a six-year whirlwind college experience, including stints at Vanderbilt University, Jagiellonian University in Krakow, Poland, and the Sorbonne University in Paris. She worked as an emergency room physician with Presbyterian Healthcare Services for 20 years.
Abner ”Marty” Martin Landry III, MD (Resident - Diagnostic Radiology), died peacefully on July 18, 2021, following a month-long battle in the ICU. He was a practicing radiologist in New Orleans before moving to Clearwater, Fla. and continuing his practice at Largo Medical Center as chief of Radiology. He spent countless hours providing medical care at the Clearwater Free Clinic, volunteering for Doctors Without Borders and at the Belize Food Bank, and tirelessly supporting efforts to make universal health care a reality in the United States.
Jimmie “Jim“ Reed, MD (Resident - Internal Medicine), died at his home on August 4, 2021. He was inducted into the U.S. Army and earned his parachutist badge before being honorably discharged in 1958. He served as director of radiology for Brownfield Regional Medical Center in Brownfield, Texas, and as clinical assistant professor of Radiology at Texas Tech. He operated a private dermatology practice from 1991-2004, later combining his practice with radiology from 1998-2004. Reed returned to his hometown in 2005, where he continued to work in radiology until his death.
Armin Rembe, MD (Resident – Hematology), died on April 25, 2021, surrounded by his loving family at their home, the historic Los Poblanos Ranch in the Village of Los Ranchos, N.M. The first oncologist-hematologist in Albuquerque, Rembe was devoted to his patients and their families throughout his career, often making house calls and even trading care for lambs and chickens. Retiring from medicine, he started a second career as "Farmin' Armin," growing organic vegetables and eventually lavender as part of a project to both perpetuate farming in the Rio Grande Valley and minimize water use in agriculture.
Marc Edward Ritsema, MD (Resident – Psychiatry; Fellow - Child Psychiatry), died on March 9, 2021. His career as a physician took him from Michigan to New Mexico to Massachusetts before settling in Milwaukee, Wisc,. to raise his daughters as a single parent. In private practice throughout his career, he was also on the clinical faculty of the University of Wisconsin School of Medicine and Robert Wood Johnson Medical School. He took great pride in caring for children..
Faculty
Lawrence “Larry” A. Osborn, MD, died unexpectedly on March 13th, 2021. He spent most of his career as an interventional cardiologist at UNM, where he started the coronary angioplasty program in 1987. Though he was passionate about academic pursuits and published many peer-reviewed articles and book chapters, he spent the majority of his career on what he valued above all else: patient care and teaching residents and fellows.
Pratap S. Avasthi, MD, died at his home in Albuquerque on January 12, 2021 at the age of 85. Although he suffered his first heart attack at age 36 and battled chronic cardiac issues, his perseverance and curiosity sustained him for nearly 50 additional years. He immigrated to Albuquerque in 1966 from India to pursue a residency in internal medicine at UNM. He spent most of his career teaching and training UNM medical students, conducting research related to renal diseases and treating patients with kidney ailments. After retiring in 1996, he continued to pursue his lifelong interest in the sciences, especially in the fields of astrophysics and space exploration.
Thomas J. Carlow, MD, died on March 15, 2021. He spent a long and fruitful career as a neuro-ophthalmologist in Albuquerque – and was the only one in New Mexico for 30 years. A pioneer in his field, he started an annual medical meeting, the North American Neuro-Ophthalmology Society, which became an international society. He also served in the U.S. Army Public Health Service. He derived great pleasure teaching residents in neurology, ophthalmology and neurosurgery.
Gary Peterson, MD, died following a battle with idiopathic pulmonary disease on September 9, 2021, at his home in Chapel Hill, N.C. Peterson was a research fellow at the Biological Sciences Research Center at UNC-Chapel Hill, and then ran the Child Psychiatry Unit at UNM for five years. He later joined the Southeast Institute for Group and Family Therapy in Chapel Hill, where he continued in private practice for the remainder of his career.
Paula Jean Clayton, MD, died peacefully on September 4, 2021, surrounded by loved ones. In 1980, she became the first woman in the United States to chair a department of psychiatry, joining the University of Minnesota Medical School, a role in which she served until 1999. She subsequently moved to Santa Fe and became a professor of Psychiatry at the UNM School of Medicine from 2001 to 2005. In 2006, she moved to New York City to become the medical director of the American Foundation for Suicide Prevention. Throughout her career, Clayton remained committed to advancing the field of psychiatry, conducting research, teaching, mentoring young doctors and seeing patients..
Transformation in Times of COVID
On March 14, 2020, there was heavy traffic everywhere in Quito, Ecuador, when, at 9:35 a.m., all the local radio stations broadcast a news bulletin: “The city will be closing down, curfew is instituted starting at 3 p.m.”
I did not care about the news. I was frantically driving home to check my email. It was Match Day, and my future as a medical professional was on the line. I arrived home, rushed inside, leaving my my front door open.
I turned on my laptop and there it was, the dreaded message, “We are sorry you did not match to any position.”
The rest of the day is a blur. I was discombobulated, with many thoughts in my head as I prepared for the curfew. I don’t recall much more about that week – long story short, I was not able to match, which led me to believe that this was the worst week of my professional and personal life.
The news hit hard. On the one hand, my dream of becoming a resident in the U.S. was fading, and on the other, a once-in-a-lifetime pandemic was upon us. My options looked bleak, I had no compass. I tried to bounce back as best as I could, but opportunities were not ample.
READ
MORE

CLOSE
Transformation in Times of COVID
By David A. Andrade, MD - PGY I Psychiatry Resident
On March 14, 2020, there was heavy traffic everywhere in Quito, Ecuador, when, at 9:35 a.m., all the local radio stations broadcast a news bulletin: “The city will be closing down, curfew is instituted starting at 3 p.m.”
I did not care about the news. I was frantically driving home to check my email. It was Match Day, and my future as a medical professional was on the line. I arrived home, rushed inside, leaving my my front door open.
I turned on my laptop and there it was, the dreaded message, “We are sorry you did not match to any position.”
The rest of the day is a blur. I was discombobulated, with many thoughts in my head as I prepared for the curfew. I don’t recall much more about that week – long story short, I was not able to match, which led me to believe that this was the worst week of my professional and personal life.
The news hit hard. On the one hand, my dream of becoming a resident in the U.S. was fading, and on the other, a once-in-a-lifetime pandemic was upon us. My options looked bleak, I had no compass. I tried to bounce back as best as I could, but opportunities were not ample.
I tried to become a part of the pandemic relief efforts in my country and in the U.S. I wrote letters to the U.S. embassy and several hospitals in New York City, where the pandemic hit the hardest. I was rejected everywhere, but the toughest part was being denied opportunities by my own country. Every one of those responses sounded the same to me: “Sorry, if you are not good enough to match, you are not good enough for this, either.”
In the meantime, I tried my best to keep occupied with “pandemic chores,” making sure my family was safe during those trying times. Mentally, I tried to focus on a new objective, but it was unclear what that might be. The 2021 Match? Restarting my career in my home country? Or trying to do so in a different one?
While still thinking about my future, I got involved working remotely as a clinical consultant with a mental health institution in Albuquerque. but I was still preoccupied about my next steps.
I was positive that my future lay in the U.S., and as soon as borders were open, I tried to get into the country to improve my chances for the 2021 Match.
But U.S. Customs and Border Protection had different plans. They detained and questioned me for several hours on the suspicion I was coming to work illegally in the country. After an exhausting interview – and by what I can only call divine intervention – I was able to come into the country for 30 days, one-third of the intended time.
This was the turning point. After a few drinks and a psychotherapy session that made me realize I had acute stress disorder, I decided that it was enough. As a medical professional, I was used to the false belief that I was in control, but after everything that happened, I decided I did not have control – and that was OK. I decided to let go and think about everything as a blessing. I made the best out my short-lived clinical experience, went back to Ecuador, enjoyed quality time with my family, continued to work remotely, got married and applied to the 2021 Match with more faith than conviction.
I did it. I MATCHED IN PSYCHIATRY!
When people say that the pandemic changed their lives, it is probably true. Everyone had to adjust to unprecedented circumstances. Now, the question is, is this lasting change or not? For me, it was.
The year 2020 was professionally disastrous, but I learned the most important lesson, to not hold on too tightly, to enjoy the moment, even in the worst of circumstances and to think about everything as a learning experience.
As you can see, 2021 has been the opposite, and I am glad. 2020 will always hold a special place in my memory. It will be known as the year I started to enjoy life instead of trying to control it.
LTSS
giving levels
Any gift in any amount to a School of Medicine scholarship fund is valued and recognized by the La Tierra Sagrada Society. Donors to LTSS for any of these scholarships are called “Supporting Donors.”
With an annual gift of $1-$999, you will be listed as a Cherry Donor in the scholarship dinner program. CLICK TO JOIN

With an annual gift of $1,000- $2,499, you will be listed as a Turquoise Donor in the scholarship dinner program.
CLICK TO JOIN

With an annual gift of $2,500-$4,999, you will be listed as a Silver Donor in the scholarship dinner program. CLICK TO JOIN

With an annual gift of $5,00-$24,999, you will be listed as a Gold Donor in the scholarship dinner program. CLICK TO JOIN

With a gift of $25,000 or greater, you establish a named endowed scholarship to be awarded annually and you will be listed in the scholarship dinner program as an Endowment Donor. CLICK TO JOIN

Any Scholarship. Any Amount.
La Tierra Sagrada is the largest scholarship entity at The University of New Mexico School of Medicine.
Committed to recognizing all who support scholarships at the School of Medicine, the La Tierra Sagrada Board of Directors is pleased to announce. . .
When you GIVE,
you BELONG.
Now, when you give to any UNM School of Medicine scholarship, you will belong to La Tierra Sagrada.
READ
MORE
SERVE THE PRESENT. SHAPE THE FUTURE.
La Tierra Sagrada is the largest scholarship entity at The University of New Mexico School of Medicine.
Committed to recognizing all who support scholarships at the School of Medicine, the La Tierra Sagrada Board of Directors is pleased to announce. . .
When you GIVE,
you BELONG.
Now, when you give to any UNM School of Medicine scholarship, you will belong to La Tierra Sagrada.
 PLEDGE "25"
PLEDGE "25"
Since 1996, the La Tierra Sagrada Society has awarded $1.7 million in scholarships and research grants. $1.2 million has gone directly to students through scholarships.
Make your impact and celebrate the 25th Anniversary of La Tierra Sagrada by Pledging “25.”
Give a one-time gift of $25, $250, $2,500 or a $25,000 endowment.
Faculty and staff donors are encouraged to consider giving a recurring “25” gift via payroll deduction.
For membership information, please contact Erika Anderson at 505.272.1913 or EMAnderson@salud.unm.edu
give online at: goto.unm.edu/ltss25
CLOSE
Editorial Board & Contributors
managing editor
Ashley Salazar
creative director
Bridgette Wagner Jones
READ
MORE

CLOSE
Editorial Board & Contributors
managing editor
Ashley Salazar
creative director
Bridgette Wagner Jones
editors
Alexandria Sanchez, Elizabeth Sandlin
contributing writers
David A. Andrade, Supreetha Gubbala, Tenisha Marques, Ruth Morgan, Paige R. Penland, Michael E. Richards, C. Nathaniel Roybal, Ashley Salazar, Alexandria Sanchez, Maggie Schold, Michele W. Sequeira
graphics & layout
Bridgette Wagner Jones
photography
Jett Loe, Raymond Mares, José Rodríguez, Ashley Salazar, Allan Stone
dean’s office
Michael E. Richards, MD, MPA
Interim Dean, UNM School of Medicine
contact
UNM School of Medicine
Office of Advancement & Alumni Relations
MSC08 4720 Fitz Hall Rm 182B
1 University of New Mexico
Albuquerque NM 87131-0001
505.272.5112
subscription information
unmsomalumni@salud.unm.edu
editor email
asmsalazar@salud.unm.edu
We welcome the submission of stories, photographs and letters to the editor.
UNM Medicine is published by the UNM School of Medicine Office of Advancement and Alumni Relations
Printed in the USA Copyright 2021
The University of New Mexico Health Sciences Center