Pediatric and Adult Infectious Diseases in Africa


Perhaps one of the most intriguing aspects of Plasmodium falciparum malaria is the diverse clinical presentations of severe disease. In areas of holoendemic P. falciparum transmission, the clinical presentation of severe malaria is predominantly severe malarial anemia, often accompanied by respiratory distress. This condition most commonly occurs in infants and young children less than 5 years. The prevalence of cerebral malaria in areas with high rates of falciparum malaria is typically very low. Conversely, in areas with seasonal and/or low levels of P. falciparum transmission, severe malaria can present as a combination of clinical features, including malarial anemia, cerebral malaria, and respiratory distress.
Human malaria, transmitted by female Anopheles mosquitoes, is a protozoan disease typically caused by one of four members of the genus Plasmodium falciparum, vivax, ovale, and malariae.
Malaria is one of the leading causes of morbidity and mortality of infectious disease origin throughout the world, resulting ~228 million clinical cases per annum and ~ 405,000 deaths with children under 5 years representing 67% (272,000) of the malaria mortality. Over 93% of the malaria cases and 94% of the deaths occur in sub-Saharan Africa, with immune-naive children under 5 years having the majority of the disease burden. Malaria-related morbidity and mortality in African children is largely due to infection with falciparum. Severe clinical manifestations of falciparum malaria typically include one or more of the following: hypoglycemia, hyperparasitemia, cerebral malaria, malarial anemia, and respiratory distress. Among these disease sequelae, malarial anemia is responsible for the greatest amount of malaria-related morbidity and mortality worldwide. When hemoglobin levels become profoundly low (Hb<5.0 g/dL), life-threatening severe malarial anemia (SMA) can result. SMA in African children is often a multi-factorial disease due to the presence additional anemia-promoting factors, such as nutritional deficits and co-infection with other pathogens (e.g., hookworm, bacteremia, HIV, and tuberculosis), making the etiological basis of malarial anemia complex. As such, when investigating malarial anemia it is important to carefully define the diverse factors that can contribute to reduced hemoglobin levels. We have been investigating the pathogenesis of malarial anemia and related co-infections in infants and young children in western Kenya for the past 18 years.

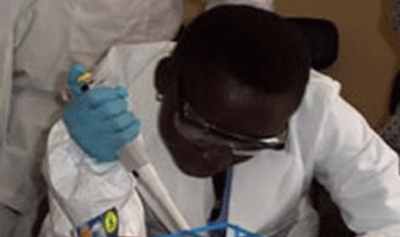
Microbiology laboratory at the UNM-Kenya facilities in Siaya Because bacteremia (blood borne bacterial infection) is common in sub-Saharan Africa, it represents an important source of morbidity and mortality in infants and children. In western Kenya, there is a high rate of co-infection with bacteremia and malaria that enhances severe disease outcomes greater than witnessed in either disease alone. At Siaya County Referral Hospital, we established a microbiology facility to diagnose bacteremia through traditional microbial cultivation and molecular methods. In addition, we perform antimicrobial susceptibility testing through standard and molecular methods. These activities aid in clinical management and have improved patient outcomes, as well as providing a platform of training scientists in Kenya. The ongoing activities are also aimed at mitigating the high rate of antimicrobial resistance in the region.

Upon implementation of our activities in western Kenya, nearly two decades ago (2002), there was a high prevalence of HIV/AIDS in the pediatric population, which remains challenging elevated to date. Since one of the primary clinical hallmarks in untreated pediatric HIV is anemia, our laboratories investigate the important influence of HIV-1 as a co-factor in the etiology of childhood anemia. Although some earlier research findings suggested that the interaction between malaria and HIV-1 was minimal, our studies have identified novel molecular pathways that exacerbate morbidity and mortality in co-infected children
Since there is presently no widely available standard-of-care efficacious vaccine for malaria, development of a vaccine that protects against the development of malarial anemia is an important step in preventing the morbidity and mortality associated with the disease.
A comprehensive understanding of malaria that accounts for the complex genetic, inflammatory, and clinical factors associated with the disease could be used to better predict disease outcomes. This information would be extremely valuable for designing novel vaccines, evaluating the immune response, and identifying at risk groups for enhanced therapeutic intervention. The primary goal of our studies in western Kenya is to gain a better understanding of the genetic and immunological factors that drive enhanced morbidity and mortality in pediatric populations with malaria and other common endemic infections.
Currently, the primary treatment interventions for the management of severe malarial anemia are the use of antimalarial drugs, blood transfusion, fluid replacement, and empiric treatment with broad spectrum antibiotics to cover the potential of undetected bacterial pathogens. We have active investigations on identifying novel antimalarial drug regimens and are developing novel molecular diagnostics to rapidly detect bacterial pathogens. Collectively, these activities are aimed at meeting the challenge of antimalarial drug resistance and may help to mitigate the spread of antimicrobial resistance associated with empiric antibiotic treatment.

SARS- Cov-2/COVID 19
Publications