Program Model
The Pathways to a Healthy Bernalillo County program was highlighted in the Federal Agency for Healthcare Research and Quality's (AHRQ) Innovations Exchange website as an innovative program that reduces health disparities. The AHRQ web site has a full profile, which has been updated each fall for the past 3 years.
Summary
"The Pathways to a Healthy Bernalillo County Program uses a version of the Pathways Model to identify vulnerable, underserved residents and connect them to health and social services. Clients are identified through interagency referral among the program's network of 13 community-based organizations. Community health navigators help clients access additional health and social services, assist with coordination of care, and monitor client progress. Participating agencies receive payments based on their ability to identify at-risk clients, connect them with needed services, and achieve positive outcomes, while a central hub and database help coordinate client services. The program has enhanced access to needed services for many of the more than 3350+ unduplicated clients served in its first 6+ years of operation, with more than 1760 completing all their pathways and exiting the program; by program design, each completed pathway indicates a successful outcome."
Who is the Pathways client?
Pathways targets difficult-to-reach populations in the County which include, but is not limited to low income, uninsured adults who may be experiencing one or several of the following:
- Have multiple or complex unmet needs and reports feeling unhealthy
- Have had a minimum of one Emergency Room visit within the last year
- Currently experiencing homelessness and disconnected from services
- Urban off-reservation Native American not connected to or trusting of the currently existing resources in Bernalillo County
- Undocumented and/or limited-English proficient (LEP) immigrant who does not understand how to access existing resources and/or have run into barriers trying to navigate the system
- Hungry and averaging less than two full meals per day
- Any of the above who are parenting young children
Pathways is designed to target key risk factors which include:
- Poverty
- History of incarceration
- Culture: fear and dislike of system; ineffective use of community resources.
- Self-reported poor health
- Lack of an established medical home
- Using the Emergency Room for non-emergency situations
- Transportation barriers
- Housing instability
- Lacking I.D. cards
- Behavioral health needs
- Lacking dental care
- Limited English proficiency
- Unemployment
- Lacking health insurance
Example of a client on pathways
What is a pathway?
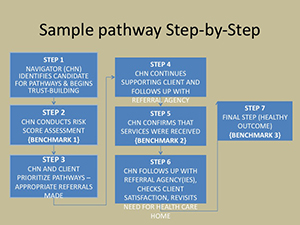
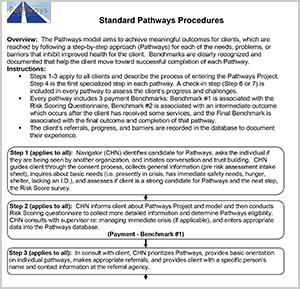
Pathways are specific to prioritized needs that a client has identified. For example, one pathway or need for a client may be to find housing; another to establish a medical home; and another to go back to school to obtain a GED. With the help and guidance of a Navigator, clients pick their pathways and work toward completing each one. A pathway begins with the identified problem and several action steps, leading to meaningful outcomes for the client. Critical benchmarks along everypathway include the risk assessment, an intermediate action step that marks some success toward completing the pathway, and a completed pathway.
Step by step description of pathways
Reaching outcomes
Outcomes are reached when clients successfully complete their different pathways.
Examples of pathways used in our project with identified outcomes.
Who drives the model?
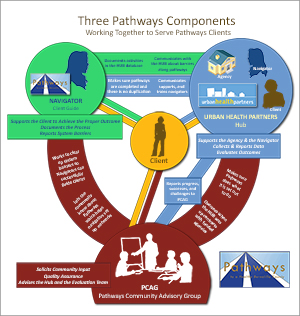
The key to the success of this model is an extensive care coordination network. Quality performance and preventing duplication are priorities. We do this through:
- Community Health Navigators (Navigators):
- May also be referred to as a Promotor/a, Community Health Worker, Case Manager, Outreach Worker or Community Liaison.
- Work at a community agency that receives pathways funding.
- Finds individuals most at-risk and works with them to assess their needs.
- Guides individuals (the client) through a series of steps (Pathways) to mark their progress toward improved health and well-being (health outcomes).
- Reports system barriers that are encountered while guiding clients.
- Documents all activities in the pathways database.
- Hub:
- Central support system (through UNM Health Sciences Center Community Health Initiatives under the Office for Community Health) for the contracted community-based organizations and their Navigators.
- Provides ongoing communication, support, and training to the Navigators.
- Maintains and monitors program database for program implementation and evaluation purposes.
- Confirms that Pathways are completed and that there is no duplication of clients across pathways partners.
- Prepares reports for the UNM Hospital, the Bernalillo County Commission, and the general public.
- Conducts annual Report-to-the-Community
- Pathways Community Advisory Group (PCAG):
- Serves as an external advisory committee to the Hub
- Raises community awareness about the pathways model
- Works with Hub on strategies to effectively reduce systems barriers.
National Models
The Community Health Access Project (CHAP) in Richland County, Ohio serves as the original Pathways model from which all others evolved. Drs. Mark and Sarah Redding, both physicians, initiated this model in Ohio in 1999, which was based on their prior experiences working with Community Health Workers in remote areas of rural Alaska as physicians with the Indian Health Service (IHS). Their personal experiences in Alaska with the IHS led to the creation of the Pathways care coordination model, which has since been replicated in more than sixteen different geographic areas across the U.S. Link to: AHRQ Innovation Profile.
Summary
"The Community Health Access Project (CHAP) implemented the Pathways Model, which employs community health workers who connect at-risk individuals to evidence-based care through the use of individualized care pathways designed to produce healthy outcomes. This model promotes timely, efficient care coordination through incentives and prevents service duplication through use of a Community Hub, a regional point of patient registration, and quality assurance supporting a network of agencies involved in providing care to the target population. The first implementation of the model in Richland County, OH, resulted in increased services to at-risk women and a decline in the rate of low birth weight babies."
The Muskegon Community Health Project developed a pathway that uses medical navigators to help newly released or paroled prisoners obtain their medical records, find a medical home, and access needed primary care and specialty services. The health navigation program began in Muskegon County and serves two neighboring counties in Michigan. Link to: AHRQ Innovation Profile.
Summary
"The Michigan Prisoner Reentry Initiative, a statewide initiative through 18 regional sites that cover all 83 Michigan counties, helps newly released prisoners access services needed to facilitate successful reentry into the community. The Muskegon Community Health Project participates in the local implementation of the initiative by helping prisoners access health services. The Community Health Project has accomplished this through implementation of the Pathways model, a model that involves “pathways” of action steps implemented by community health workers who connect at-risk individuals to care. The health project’s pathway links newly released prisoners to a medical home, helps them access needed medications and primary and specialty care, and ensures that they obtain their medical records on release from prison. The program appears to have been a contributing factor to a significant decline in recidivism rates in Muskegon. Without the program, more than 2,500 individuals (mostly men) who went through the pathway would have been returned to the community without access to medical support services. (Note that the state of Michigan reorganized and transitioned the program as of December 31, 2013; services are now delivered internally by the Michigan Department of Corrections.)"