Learn complex procedures using state-of-the art equipment. Submit your application today.
 505- 272-2610
505- 272-2610
The University of New Mexico School of Medicine is home to a Basic and Advanced Trauma Computer Assisted Visual Experience (BATCAVE) healthcare simulation program. This multidisciplinary educational tool is dedicated to improving assessment, procedural skills and patient management. BATCAVE enhances overall competency at all levels of patient care.
The Department of Anesthesiology provides a robust simulation experience for training its residents. Starting in the PGY-1 year, residents partake in an introductory Airway Workshop that emphasizes the basics of airway management.
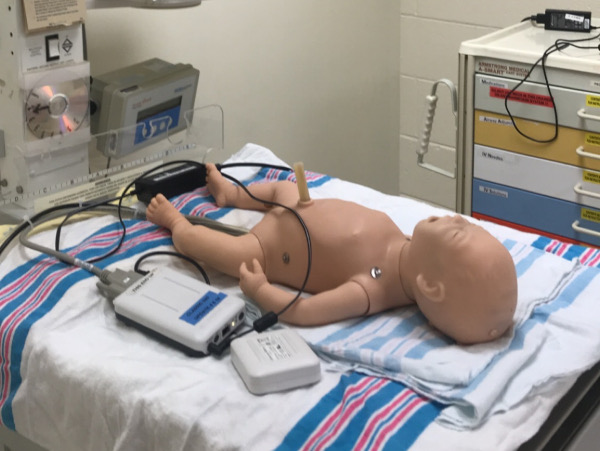
Multiple types of simulation mannequins are utilized, and an instructor to learner ratio of 1:4 allows for focused education on correct technique and appropriate reasoning processes.
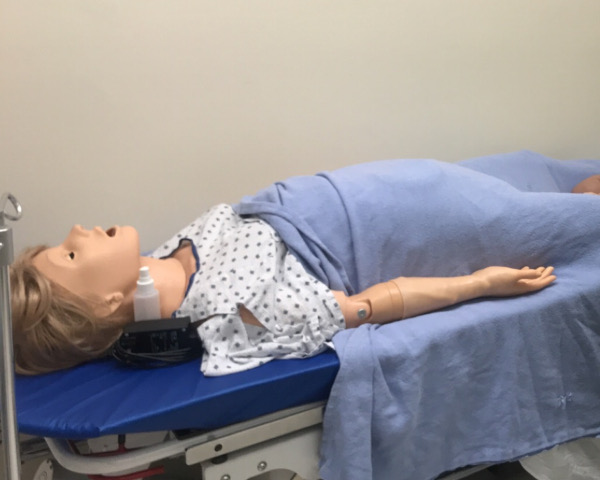
In the CA1 year, residents are exposed to simulation every week for the first two months. Such tasks as room setup, machine troubleshooting, rapid sequence intubation, maintenance and emergence are practiced. As the residents develop comfort with the new environment, common urgencies such as hypoxia, tachycardia and arrhythmia are added to scenarios. Advanced Cardiovascular Life Support (ACLS) is reviewed and practiced in this controlled setting.
Each resident spends two hours practicing Ultrasound Guided Central line placement and receives feedback and competency validation at the start of CA1.
From that time forward, simulation is used to model rare, life threatening perioperative emergencies. Residents work together in teams of two while two attendings create the simulation, making use of high-fidelity monitors and mannequins. Standardized patient actors are included in scenarios to develop specific communication skills that are rated as they would be on the Anesthesia Boards, but in this formative setting. Vascular, lung and abdominal ultrasound, along with bronchoscopy, transthoracic and transesophageal echo simulators add a dimension of skills performance to specific emergency scenarios. The debrief of each scenario stresses the values of differential diagnosis development, critical thinking, and team-based communication skills.
Each year, the department creates a unique seven station Object Structured Clinical Examination (OSCE) test in which the residents simulate the experience of taking this portion of the Anesthesia Boards.
The residents are “graded” as they would be in real life and given specific feedback regarding strengths and weaknesses revealed in this mock “high stress” offering.
Supporting the OSCE experience are modules developed by faculty that drill communication skills in difficult circumstances: providing bad news, disagreeing with a colleague, negotiating issues of autonomy, and others. These modules make use of professional medical actors, and slow down the process to help the resident to understand the components involved in successful communication, even in awkward situations.
Throughout the year additional simulation experiences related to airway management (including ENT– and Anesthesia–led cricothyrotomy training) and Point-of-Care Ultrasound are mixed into the residents’ learning experience.
The protected environment of simulation is a fantastic place for residents to “learn by doing,” and to allow the scenario to create a degree of stress that is both conducive to learning and allows for significant reflection, self-improvement and self-actualization.
Education and Development Manager
Yow Feng
yfeng@salud.unm.edu
Department of Anesthesiology & Critical Care Medicine
UNM Hospital
2211 Lomas Blvd NE
Albuquerque, NM 87106